Source: The Conversation (Au and NZ) – By Kadir Atalay, Associate Professor in Economics, University of Sydney

A cancer diagnosis is frightening news for anyone. But our fresh analysis shows what happens next can depend on how much money you have and where you live.
Among middle-aged Australians cancer is the leading cause of death, accounting for 45% of all deaths among those aged 45 to 64 years.
In an article just published in Health Economics, we examine the inequality in mortality (or death rates) across Australia. As has been found elsewhere, death rates in Australia are highest among those with the lowest socioeconomic status (SES).
This measure of income, employment and education has long been recognised as related to both a person’s health status and their ability to “buffer” against the negative impacts of a health condition.
What’s new from our study is our finding middle-aged men living in the poorest local areas of Australia in 2016-18 were twice as likely to die from cancer than those living in the richest areas. Women in the same areas were 1.6 times more likely.
This disparity between rich and the poor is growing over time, widening by 34% from 2001 to 2018. And while deaths from cancer have fallen everywhere over time, they have fallen by more in our richest locations compared to our poorest.
Measuring death and status
For our new analysis, we examined all deaths and those from specific causes for men and women across all age groups. We used death registry data provided by the Australian Institute of Health and Wellbeing and Census data on SES.
We ranked local areas across the country by two measures of SES: the Australian Bureau of Statistics’ Index of Relative Socio-economic Disadvantage and the share of households in a local area living in poverty (sourced from a customised Census report). Our findings remained consistent using either of these measures.
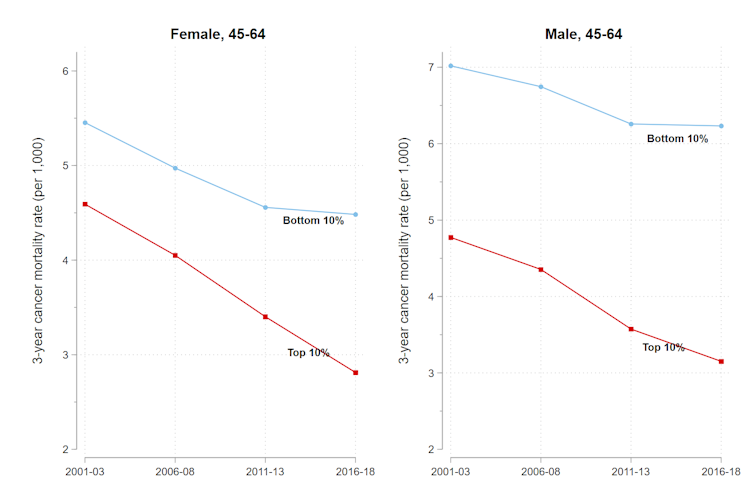
The new findings for middle-aged Australians stand out because inequality in mortality has been relatively stable over time and death rates are falling for most other age groups.
Among young Australians aged 15–24 years we can see death rates falling and the SES gap in mortality shrinking due to greater declines in road deaths in poor areas.
Nevertheless, if we could eliminate death inequality, and all Australians under the age of 75 enjoyed the lower mortality rates of those living in our most socioeconomically advantaged areas, 28% of the all deaths across Australia could have been avoided.
Read more:
What actually is palliative care? And how is it different to end-of-life care?
Why the gap?
We also looked at what could be driving this rising inequality in mortality for middle-aged Australians. Our research suggests different access to health care may have a role to play. Two findings support this.
First, when we compare city areas to more regional and remote areas, we find the increase in inequality (between low and high SES) is not as strong for women and is not present for men. This suggests the widening gap is because of smaller declines in deaths over time in our poorest regional and remote areas. In other words, improvements have been slower there.
Second, over the period from 2001 to 2018, the number of doctors per person is consistently greater in richer regions than poorer regions of Australia.
Over the past 20 years there have been substantial technological advances in medicine. However, access to new medications and treatments is often only available following consultations with primary physicians (such as GPs) or specialists.
Inequality in access to health care – as we can see exists between wealthier cities and poorer regional and remote areas – is likely to lead to a different level of benefit from medical advancements between the rich and the poor.
For cancer in particular, one of the contributing factors to disparities in cancer deaths by SES is the limited availability of screening and treatment options.
We can’t say for certain poverty and access to doctors are linked with poor health outcomes and higher death rates, but it certainly warrants attention from policymakers.
More analysis needed
Accessibility to health care significantly influences disparities in cancer death rates. But we need more comprehensive analysis of how various social determinants of health contribute to these inequalities.
These could include social and environmental characteristics of local areas, health behaviours and cancer awareness, income or income inequality. Future research should examine whether the socioeconomic disparities in cancer death rates are also evident in cancer diagnoses.
It’s also important to explore how population screening programs (such as BreastScreen Australia and the National Bowel Cancer Screening Program for over 50s) and subsidised early detection initiatives (including Medicare-subsidised breast cancer imaging and prostate-specific antigen tests) can mitigate these disparities.
Lastly, policymakers should be alert to the possibility delays in screening and changes in health-care accessibility related to the COVID pandemic may have exacerbated these health inequalities.
Read more:
How your status, where you live and your family background affect your risk of dementia
![]()
Research for this article was supported by a grant from the ARC Centre of Excellence for Children and Families over the Life Course and a 2020 SOAR fellowship from the University of Sydney. Kadir Atalay does not work for, consult, own shares in or receive funding from any other company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Research for this article was supported by a grant from the ARC Centre of Excellence for Children and Families over the Life Course and a 2020 SOAR fellowship from the University of Sydney.
Rebecca Edwards does not work for, consult, own shares in or receive funding from any other company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
– ref. Poor, middle-aged Australians are more likely to die from cancer – and the gap is widening – https://theconversation.com/poor-middle-aged-australians-are-more-likely-to-die-from-cancer-and-the-gap-is-widening-210878







