Source: The Conversation (Au and NZ) – By Brett Montgomery, Senior Lecturer in General Practice, University of Western Australia
From August 1, if the federal government has its way, Medicare will stop paying for GPs to interpret common heart tests called electrocardiograms, or ECGs.
Health Minister Greg Hunt says the decision is based on safety advice from a top-level medical expert panel convened by the government to review Medicare rebates. But a closer look at the advice reveals the panel suggested precisely the opposite.
And by treating ECG interpretation as a specialised task rather than an everyday part of a GP’s toolkit, the change risks making it harder and more expensive for patients to access these simple but potentially life-saving tests.
What are ECGs?
ECGs are tracings of the heart’s electrical activity. If you’ve watched a medical drama on TV and seen a flat line on a screen bounce back to a healthy wobbly line as a patient is rescued from cardiac arrest, you’ve seen an example of an ECG – it’s that wobbly line.
In fact, ECGs in real life typically consist of 12 different wobbly lines (a so-called “12-lead ECG”), as the heart’s electrical activity is measured from different directions. If you’ve had one yourself, you may remember sticky patches being placed on your skin, and a tangle of wires connecting these patches to a special machine that prints out the ECG trace.Read more: Your Apple Watch can now record your ECG – but what does that mean and can you trust it?
These tests are a common tool for many doctors, including GPs. All medical students are expected to learn to interpret an ECG – it is not a test reserved for cardiologists.
There are all sorts of situations in which a GP may need to use and interpret an ECG. One obvious example is when a patient is suffering chest pain that could be due to a heart attack or angina. Others include assessing unusual heart rhythms, such as atrial fibrillation, which is a common and important risk factor for stroke that GPs are encouraged to detect and treat.
ECGs are so fundamental that Australian general practices are required to demonstrate “timely access” to an ECG machine as part of their accreditation.
What is the government proposing?
Medicare has for many years funded the tracing and reporting of ECGs in general practice. The government is now proposing to remove funding of the reporting of ECGs from GPs. Funding for interpretation or reporting of ECGs will be restricted to specialists.
Under the new plan, public funding for ECGs in general practice will be restricted to producing (rather than interpreting) the trace. This is a technical task rather than a medical one, and many GPs, who rightly feel qualified to interpret ECGs, find this insulting.
More importantly, this loss of funding may harm patients. As shadow health minister Chris Bowen has explained, an increase in out-of-pocket costs to patients, or a reduction in funding to general practice, may limit availability of this important test to people who need it. There is good evidence out-of-pocket costs limit access to health care.
Read more: Six dollar co-payment to see a doctor: a GP’s view
While traces can be forwarded to a cardiologist for interpretation, this too may involve costs, and may be difficult in rural and remote areas.
The health minister’s explanation doesn’t stack up
Pressed to justify these proposals, health minister Greg Hunt this week told the ABC:
This came from a medical expert panel. It came from what’s known as the Medicare taskforce, led by Prof Bruce Robinson. It’s the highest clinical advice and it was based on safety.
A Department of Health spokesperson offered a similar line to the ABC in a news article this week.
The taskforce (formally called the Medicare Benefits Schedule Review Taskforce) has been working to reform the Medicare schedule – that is, the list of medical services funded by Medicare. This is a fine initiative, which brings evidence and expertise to the task of modernising Medicare. Appropriately, it enjoys the bipartisan support of our major parties. It is laudable when the government follows such independent expert advice.
The problem here is that, contrary to Hunt’s claim, the MBS Review Taskforce did not recommend that Medicare stop paying for GPs to interpret ECGs. On the contrary, the taskforce explicitly recommended the opposite.
The 344-page final report of the taskforce’s Cardiac Services Clinical Committee is pretty dry reading, but if you make it as far as page 200 you’ll find it acknowledges the importance of ECGs in general practice. In fact, the report explicitly proposes a new Medicare rebate to “allow all practitioners to take and interpret an ECG when clinically required”.
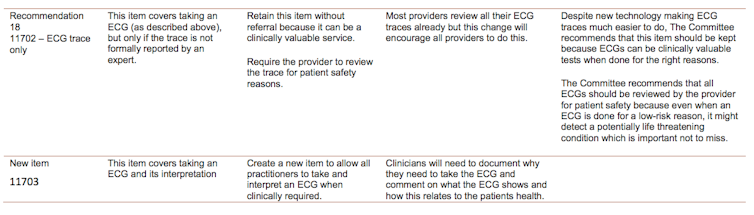
Instead, the federal government has proposed an array of new ECG rebates, none of which would fund GPs to interpret ECGs.
Read more: Explainer: what is Medicare and how does it work?
Granted, health policy is a complex area, even when there isn’t a pandemic unfolding. Nevertheless, this seems to be a clear case of expert advice not being translated into policy.
I would urge Hunt and his department to heed the advice of their own expert taskforce, and the concerns raised on behalf of GPs and their patients, and reverse their plans to defund ECG interpretation in general practice – or at least offer a full explanation as to why they are proceeding with this policy.
– ref. Why is the government restricting Medicare funds for ECGs when expert advice says exactly the opposite? – https://theconversation.com/why-is-the-government-restricting-medicare-funds-for-ecgs-when-expert-advice-says-exactly-the-opposite-143593







