Source: The Conversation (Au and NZ) – By Peter Breadon, Program Director, Health and Aged Care, Grattan Institute

GP fees are hitting more Australians than they did a few years ago. There’s a lot of talk about a crisis in bulk billing, with many people reporting they’re unable to see a doctor without paying an out-of-pocket fee.
But the biggest, most urgent problem is in the communities where most people pay fees, so called bulk-billing “deserts”. These deserts are more likely in poorer areas, so the people who most need bulk billing are missing out.
While Medicare funding changes are needed to address this problem, we also need to look at more innovative solutions. One option is for federal and state governments to step in and support or set up clinics that employ doctors, nurses and other health workers.
Bulk billing is falling, but from a historic high
The share of patients who never paid a GP fee fell from 67% in 2020-21 to 64% in 2021-22. But those rates are still high by recent standards. The rate has only fallen back to the level of 2015, and it remains much higher than a decade ago.
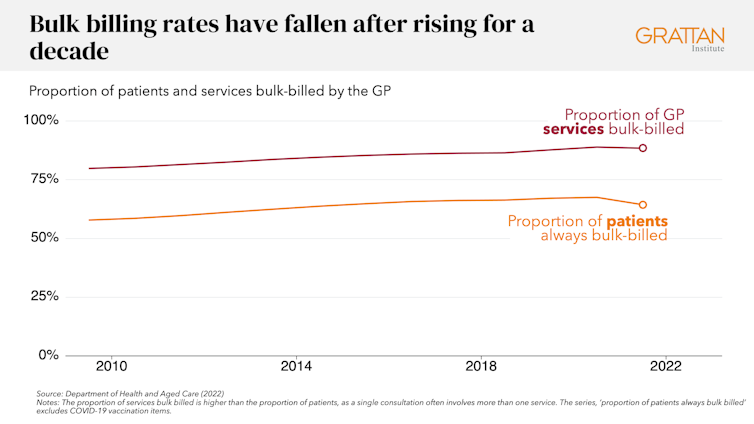
Yes, it’s troubling to see bulk billing falling, especially when fees have risen a lot. Patients who are not bulk billed now pay on average A$45 out of pocket when they see a GP. This is up 20% in real terms over the past decade.
But while the national trend is concerning, it masks a much bigger problem.
Great disparity
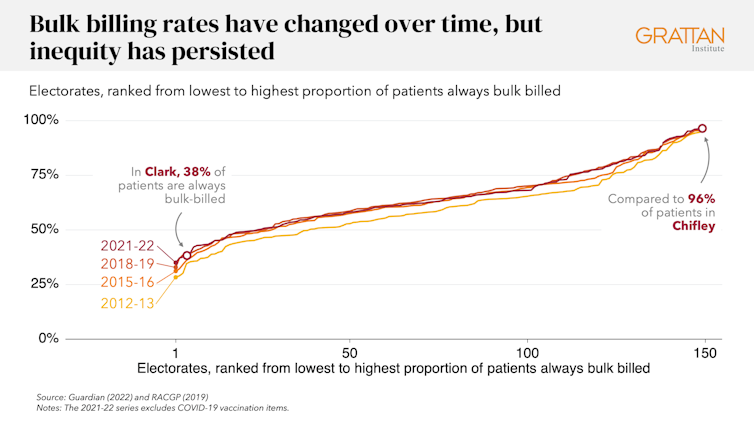
In some parts of Australia – for example, the electorates of Chiefly, Fowler, and Werriwa in outer-western Sydney – more than nine in ten GP patients are always bulk billed.
But in other parts – for example, the electorates of Canberra, and Franklin and Clark in southern Tasmania – that figure is less than four in ten.
Unlike the overall bulk-billing rate, these vast disparities have persisted for many years: the problem was just as bad a decade ago.
Bulk-billing deserts wouldn’t be such a problem if they were only in the wealthiest parts of Australia, because fees are less likely to stop wealthy people getting the care they need. But there are bulk-billing deserts in many poorer areas.
Compared to all but the wealthiest areas, the bottom fifth of electorates by income have the lowest bulk-billing rates. In 13 of the lowest-income electorates, less than 60% of patients are bulk billed.
Rural areas are worse off too: 60% of patients in rural areas are always bulked billed, compared to almost 69% in metropolitan areas.
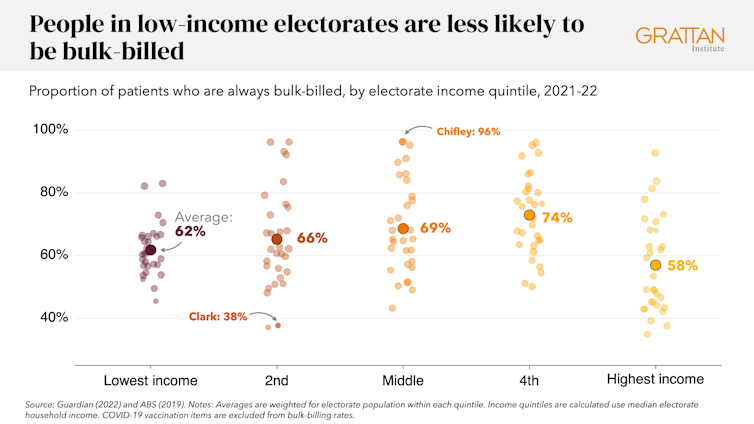
The bulk-billing deserts in poorer parts of Australia represent a serious failure of the system. Nationally, about 3.5% of people say they skip GP care because of the cost, with higher rates in rural and poorer areas. Those figures will be far higher in bulk-billing deserts, putting many people’s health at risk.
What the government should do
There have been calls to pour billions of dollars into increasing the Medicare rebate and bulk billing incentives.
But while the government should make sure payments to GPs keep up with their costs, that won’t fix the problem of bulk-billing deserts.
It might help arrest the decline in bulk billing nationally, and in some areas where bulk billing is low. But the money will mostly flow to high-bulk billing areas – it won’t do much to provide more care where there is far too little.
Read more:
General practices are struggling. Here are 5 lessons from overseas to reform the funding system
Bulk billing deserts are an enduring problem that need new solutions. To turn them around, the government must tackle two of the structural problems causing them: one-size-fits-all funding of GPs, and areas that don’t have enough health care to go around.
The government has already signalled it will develop a new funding model that pays GPs for providing ongoing care, which would improve on the current outdated and dysfunctional system. That funding should give higher payments for patients with greater need.
That would boost income for clinics with patients who need free care the most, helping those clinics to avoid charging their patients. It would be a big step in the right direction.

Shutterstock
But even then, there would still be areas without enough health-care workers to meet the community’s needs, including many rural areas, resulting in too little care, and too little bulk billing. Governments must go well beyond the Medicare rebate and other incentives to fix these broken health-care “markets”.
The federal and state governments need to step in to support existing clinics or set up new ones that employ salaried health-care workers. This support needs to be tailored to local needs. It could be employing a GP to work out of a rural hospital if there are no GPs in the area, or setting up a new community-controlled primary care service, or helping an existing clinic hire extra staff.
Rather than ad hoc announcements, there should be secure national funding for this care, targeted at the areas of greatest need – especially the poorest bulk-billing deserts.
This change should be accompanied by many other reforms to attract clinicians to areas where they’re needed most, such as further expanding new models of GP employment and training in rural areas, which give “rural generalist” doctors a single employer during their training across a range of different health settings in a region.
There should also be reforms to expand the teams supporting GPs in areas with too little care. This can reduce GP burnout, allow clinics to provide more care, and bring Australia in line with other countries. As well as administrative, allied health, pharmacist and other roles, some teams could include physician assistants, who work under the supervision of a doctor and can provide the full range of services a doctor provides.
One test for next month’s federal budget is whether it funds solutions to bulk-billing deserts – an enduring injustice in our health-care system.
Read more:
Medicare reform is off to a promising start. Now comes the hard part
![]()
Peter Breadon’s employer, Grattan Institute, has been supported in its work by government, corporates, and philanthropic gifts. A full list of supporting organisations is published at www.grattan.edu.au.
Lachlan Fox’s employer, Grattan Institute, has been supported in its work by government, corporates, and philanthropic gifts. A full list of supporting organisations is published at www.grattan.edu.au.
– ref. If you live in a bulk-billing ‘desert’ it’s hard to see a doctor for free. Here’s how to fix this – https://theconversation.com/if-you-live-in-a-bulk-billing-desert-its-hard-to-see-a-doctor-for-free-heres-how-to-fix-this-204029







