Source: The Conversation (Au and NZ) – By Peter McIntyre, Professor, Department of Women’s and Children’s Health (Dunedin), University of Otago

Guo Lei/Xinhua via Getty Images
As the New Zealand government reviews mask mandates and other pandemic measures this week, we argue it’s time to reconsider the overall COVID strategy.
With the arrival of Omicron, the pandemic landscape has changed worldwide. Omicron’s latest BA.5 variant now dominates and, in the second half of 2022, most people in all countries have acquired immunity either from vaccination or infection, or both.
In countries like New Zealand, which are emerging from a “zero COVID” elimination strategy, governments must make the difficult transition to community transmission, particularly with respect to managing expectations.
On the one hand, a group of New Zealand public health experts recently advocated a sweeping package of measures in a strategy focused on minimising infection. This includes broadened eligibility for boosters, continued mask wearing in schools and funds to support better ventilation and extended isolation if infected.
At the other end of the spectrum is an “immunity-driven” strategy, which prioritises prevention of severe illness based on three considerations:
-
with Omicron, even those adopting the most stringent avoidance measures can be infected
-
SARS-CoV-2, the virus that causes COVID-19, is here to stay and most people will encounter it multiple times throughout their lives
-
hybrid immunity from vaccination and infection is broader and more long-lived than either alone.
Given these complexities, what are the uncertainties and trade-offs governments, the experts advising them and the public must balance? We argue it is time to focus on prevention of severe disease – and here’s why.
NZ compares favourably with other countries in the region
In June 2022, the World Health Organization (WHO) revised its global COVID-19 vaccination strategy. This included an aspirational goal of 100% vaccination of healthcare workers and adults over 60.
New Zealand is close to this goal. For people over 65, two-dose coverage is above 95% and first booster coverage above 80%. Fewer than 5% of those eligible for their first booster are yet to receive it. For health care workers, booster doses remain mandatory so current employees have full coverage.
For people older than 65 and living in residential aged care, New Zealand achieved 89% booster coverage by mid-February 2022. This head start pre-Omicron is likely to be the most significant contributor to New Zealand’s globally almost unique lower than expected total number of deaths from any cause in the two years before July 2022.
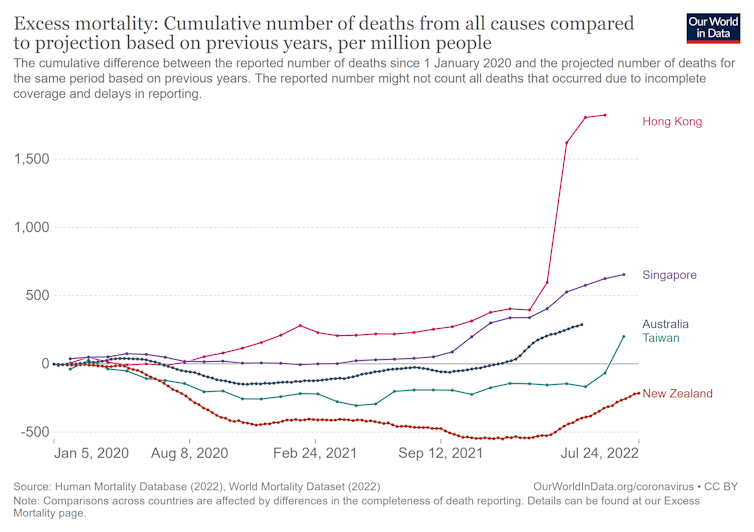
Our World in Data, CC BY-ND
In stark contrast, other countries in the Asia Pacific region with similarly stringent non-pharmaceutical measures at the onset of Omicron had much higher excess mortality. This includes Australia, where booster coverage in aged care was below 10% in January 2022.
It also includes Hong Kong, where less than 50% of people over 70 had received two doses and suffered world-record death rates when Omicron hit; and Singapore, which has the world’s highest two-dose coverage among children aged five to 11 (above 75%) but 5% of people over 80 remained unvaccinated in August 2022.

Marc Fernandes/NurPhoto via Getty Images
More than six months into the Omicron era, more than 80% of New Zealand adults have received at least two doses of vaccine. This is among the top 25 countries worldwide. But significant coverage gaps remain for Māori adults under 50.
What about severe morbidity?
In France, during the Delta period, people with no other health conditions made up 50% overall of 28 million with two vaccine doses. But they accounted for only 10% of 5,345 hospitalisations and 2% of 996 deaths due to COVID.
The highest risk of severe disease in two-dose recipients was among people in older age groups, post transplant, on dialysis and those living with cystic fibrosis, Down syndrome, mental disability or active lung cancer. Risk increased with each additional health condition and for people in poorer areas.
Read more:
COVID: masks and free tests may not curb omicron spread – here’s what we should focus on instead
When Delta was prevalent, adults (especially people over 50) required a booster dose to maintain good protection. Post Omicron, second booster doses supplemented by early use of antivirals and prophylactic antibody therapy substantially improve protection in fully vaccinated people still vulnerable to severe disease.
What about younger, low-risk populations? In children and adolescents, the vaccine protects well against the low risk of severe disease. This direct protection should be the driver of vaccination, not transient reductions in infection in their household, school or community. We recommend regular reviews of the risk-benefit trade-offs for mask wearing in schools.
How to protect people from long COVID
Long COVID is a challenging topic, complicated by changing definitions, mixing of data from pre- and post-vaccine periods, and differences in age groups.
New research finds the risk of developing long COVID is substantially lower in the Omicron period overall. Long COVID is also substantially less common in fully vaccinated people, including healthcare workers. We do not yet have data about the risk of long COVID with hybrid immunity.
As New Zealand emerges from its Omicron peak, increasing hybrid immunity, and a good – albeit not perfect – toolbox to protect people at risk of severe disease, changes the risk-benefit balance from an indirect “minimising infection” strategy towards direct “maximising immunity” approaches.
It is time to discuss whether New Zealand is ready to measure the success of its COVID strategy by how well it prevents severe disease or wants to measure success by the number of infections of any severity. Making this decision requires critical examination of the benefits, harms and cost effectiveness of each approach.
![]()
Peter McIntyre has received funding from the Otago Medical Research Foundation and the Health Research Council as a principal investigator and is a named investigator on current grants from the Health Research Council, the National Health and Medical Research Council and the Wellcome Trust. The views expressed in this piece are his own and not those of any of the bodies he is employed by or affiliated with.
Helen Petousis-Harris has been lead investigator on research funded by GSK and COIVD-19 related research funded by the MoH. She has served on Advisory Boards for GSK, Pfizer, Seqirus, and Merck. All honoraria go to institution. She has served on COVID-19 related Advisory Groups for MBIE and the MoH. She has received major grants from US CDC for COVID-19 related research.
James Ussher is Science Director of the Vaccine Alliance Aotearoa New Zealand, which has received funding from the Ministry of Business, Innovation and Employment and the Ministry of Health. The views expressed in this piece are his own and not those of any of the bodies he is employed by or affiliated with.
The views expressed in this piece are her own and not those of any of the bodies she is employed by or affiliated with.
– ref. How should New Zealand manage COVID from now – limit all infections or focus on preventing severe disease? – https://theconversation.com/how-should-new-zealand-manage-covid-from-now-limit-all-infections-or-focus-on-preventing-severe-disease-189461




