ANALYSIS: By Matthew Hobbs, University of Canterbury; Anna Howe, University of Auckland, and Lukas Marek, University of Canterbury
Within a month of the first community exposure to omicron in Aotearoa New Zealand, the variant has already become the dominant strain of covid-19.
We are yet to see the rapid and steep rise in new omicron cases that has been predicted. This could be because of asymptomatic transmission, but it is equally likely because public health measures included in the first phase of the “stamp it out strategy” have been effective.
For now, managed isolation and quarantine (MIQ) at the border is successfully stopping hundreds of cases from entering the community.
While MIQ may soon change in purpose, border restrictions may not lift until the Omicron wave passes.
The country-wide return to red settings under the covid-19 protection framework has bought New Zealand time to learn from experiences abroad. The most challenging phase is yet to come but New Zealand could be well placed to tackle it.
The best way forward is to limit widespread transmission for as long as possible. This reduces opportunities for the virus to replicate, which is when mutations occur, potentially extending the pandemic.
What we know about omicron
Omicron is more transmissible than earlier variants. New Zealand can expect a rapid and steep rise in infections, especially as we’ve already had several potential superspreading events.
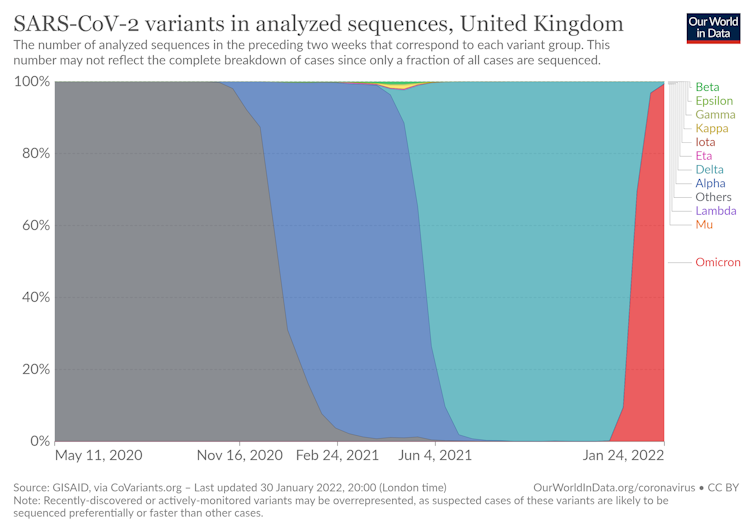
As shown below, omicron quickly replaces earlier variants.
Omicron’s transmission advantage is thought to be due to its ability to evade immunity (acquired through infection or vaccination) and quickly infect the upper respiratory tract.
The risk of reinfection also appears higher than for delta, particularly in the unvaccinated and those with lower viral loads during previous infections.
Symptoms to watch out for
Omicron symptoms include a runny nose, headache, fatigue, sneezing and a sore throat.
However, New Zealand’s high vaccination rates mean some people may not have any symptoms at all. The danger here is that they will still be able to pass on the virus to others, unaware they have omicron.
Given a choice, would you rather enter a room with Delta or Omicron?
Modeller, Professor @MichaelPlankNZ uses this scenario to explain differences between the #Covid-19 variants, while UC Health’s Dr @hobbs_PA reminds us Omicron isn’t ‘mild’. @UCNZMaths https://t.co/4dgnOSZUJC— University of Canterbury (@UCNZ) January 31, 2022
It is best to assume that any symptoms, especially a sore throat, are covid-19 until proven otherwise through a test.
For omicron, this may require saliva swab tests as recent evidence suggests they are more sensitive than nasal swabs because the viral load peaks earlier in saliva than nasal mucus.
By testing and isolating, we can avoid spreading it to others who may be at higher risk of severe illness.
Compared to delta, omicron has caused lower hospitalisation and death rates in many countries. This may be because it reproduces in the upper respiratory tract instead of the lungs.
Omicron is also meeting populations with immunity acquired through previous infection or vaccination.
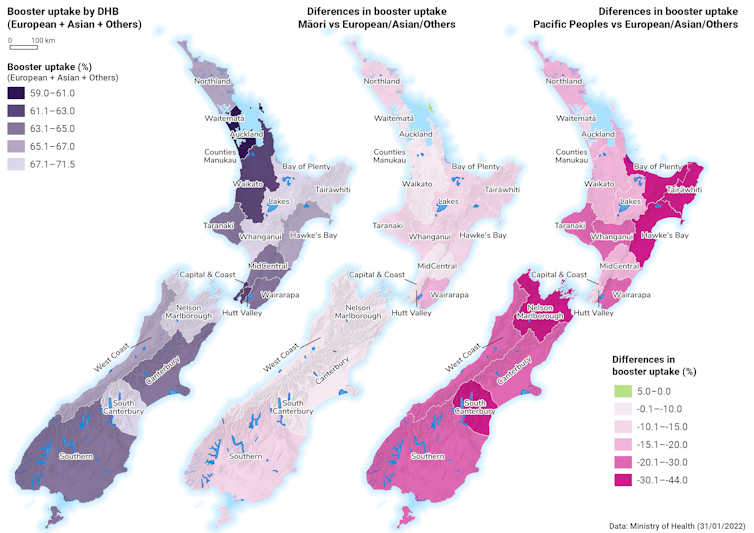
In New Zealand, 67 percent of eligible people have now received their booster, which offers high levels of protection from hospitalisation and death. Boosted individuals are up to 92 percent less likely to be hospitalised with omicron, compared with unvaccinated people.
Vaccination is especially important in New Zealand as we have had minimal prior exposure to covid-19 in the community.
Where to from here
Omicron is a “double-edged sword”. It is vastly more transmissible but less severe. However, it is not a mild infection and there is no guarantee the next variant will be less severe.
In a poorly controlled outbreak, a small percentage of a large number of cases risks overwhelming healthcare systems, increasing inequities and disrupting essential services.
This should still be true even now (with the right measures)
The kicker is that with omicron, lots of HCW sickness will drop the capacity line lower. This will be much more pronounced for the fast red surge than the slow blue wave so in fact the red surge is worse than modelled pic.twitter.com/5hfk4uSMCt— Alex Kazemi (@KazemiAlex) January 12, 2022
Healthcare workers are already over-burdened and exhausted from previous outbreaks, which have distracted from other services and exacerbated entrenched inequities.
There are several things each of us can do:
- Anybody eligible should prioritise getting boosted
- we should all continue using the COVID-19 tracer app
- we should keep indoor spaces well ventilated by opening windows and doors
- mask wearing remains important, especially where physical distancing is difficult.
- and anybody who feels unwell, should get tested and isolate.
Vaccinating children
As children return to school, we need equitable vaccinations and ventilation.
Data out of Australia indicate children aged five to 11 tolerated the vaccine well, with fewer side effects than adults.
Unfortunately, our analysis, along with other evidence, documents a concerning trend with lower childhood vaccination rates for Māori and Pasifika, as well as large variation between regions.
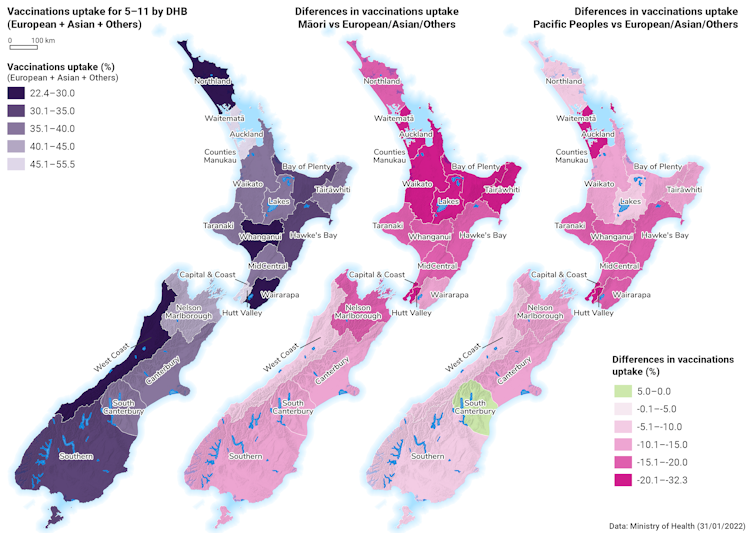
This is concerning as some countries, including the US, have seen increases in childhood hospitalisation rates for covid-19. In the UK, one in eight pupils have missed school as covid-related absences rise.
The success story of the delta outbreak
Unfortunately, there’s been little time to celebrate the rather remarkable demise of delta. Even as Auckland opened up, hospitalisations and case numbers dropped.
Summer will have helped as people spent more time outdoors. However, public health measures such as border closures, managed isolation and quarantine and contact tracing have no doubt helped stamp out much of delta, allowing a relatively normal summer holiday period for many.
Continuing to keep delta low also means we should not have to deal with a “double epidemic”.
This success may also fill us with some hope that, just perhaps, we might be able to avoid the worst of omicron during this next phase of the pandemic response, with robust and continually refined public health measures in place.![]()
Dr Matthew Hobbs is senior lecturer in public health and co-director of the GeoHealth Laboratory, University of Canterbury; Anna Howe is a research fellow, University of Auckland, and Lukas Marek is a researcher and lecturer in spatial data science, University of Canterbury. This article is republished from The Conversation under a Creative Commons licence. Read the original article.
Article by AsiaPacificReport.nz






