Source: The Conversation (Au and NZ) – By Zoë Hyde, Research Fellow, The University of Western Australia

Australia’s vaccination rollout got off to a slow start, but we’ve since become one of the most vaccinated countries in the world. More than 86% of Australians aged over 16 have received two doses, and 75% of adolescents have had their first dose. This is a fantastic achievement, but younger children are missing from this picture.
The majority of parents want to vaccinate their children. But kids aren’t yet eligible for vaccination in Australia, despite vaccines being approved for children overseas.
It’s therefore not surprising schools have become a major driver of community transmission, with unvaccinated children making up about one-third of recent cases in New South Wales.
Despite this, some state governments plan to further dismantle public health measures keeping the virus in check. In NSW, this will include scrapping mandatory mask rules.
It’s not the right time to do this while our children remain unprotected.
Additionally, the emergence of the Omicron variant, which might be more transmissible and reduce the effectiveness of our vaccines, shows Australia needs to take a much more cautious approach to easing restrictions.
COVID is not always a mild illness for kids
Adults are much more likely to experience serious illness than children, but kids are still at risk.
During the first year of the pandemic, it’s estimated that approximately one in every 400 children in the United Kingdom who got infected became sick enough to need to go to hospital, and between one in 20,000 and one in 50,000 infections were fatal.

Shutterstock.
These figures represent the infection hospitalisation rate and the infection fatality rate, and they capture the full toll of the virus, because they are based on all infections, including the asymptomatic ones that don’t get detected.
However, these estimates pre-date the emergence of the Delta variant, which causes more severe illness. Preliminary evidence from Canada suggests the Delta variant is 2.5 times more likely to lead to hospitalisation in children.
This year in Australia, 2% of detected cases in children aged 5-11 years resulted in hospitalisation, although some of these were for social reasons. These include cases in which parents were hospitalised with COVID and were temporarily unable to care for their children.
Read more:
No, we can’t treat COVID-19 like the flu. We have to consider the lasting health problems it causes
Kids can also be left with persistent symptoms (long COVID) after infection. It’s unclear how often this occurs, but in the UK, an estimated 3,000 children have been living with self-reported long COVID for at least one year.
How many children are at risk in Australia?
Because the virus that causes COVID is so contagious, almost everyone will get infected eventually if they aren’t vaccinated.
Even though only a small proportion of cases in children are severe, we can still expect a large number of children to get seriously unwell because there will be so many infections.

Shutterstock
There are 3.8 million children in Australia. If we didn’t offer them a chance to get vaccinated, based on the estimated severity of the original strain, we could eventually expect around 9,000 children to be hospitalised and 76 to 191 deaths. If we do these same calculations for the Delta variant, there could be approximately 22,000 hospitalisations in children.
The period over which this occurred would depend on the number of public health measures kept in place. COVID spread rapidly through schools in England after restrictions were lifted. By mid-October, 8% of high school students and 4% of younger children were testing positive.
Read more:
COVID-19 cases rise when schools open – but more so when teachers and students don’t wear masks
This year in Australia, 13 children and 22 adolescents have been admitted to an intensive care unit for COVID (and many more to a general hospital ward), and one child and one teenager died.
It’s unclear how many children could develop long COVID, but England’s National Health Service has had to open 15 long COVID clinics for children.
How does COVID compare to other diseases?
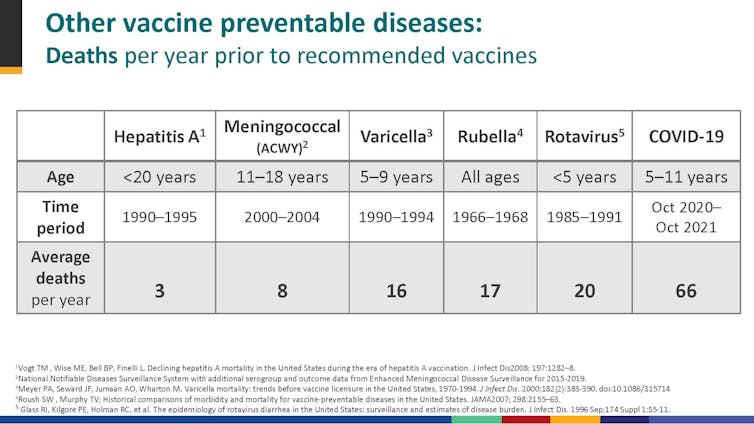
COVID is more risky for children than some other diseases that we already vaccinate against.
Today, children are routinely vaccinated against varicella (chickenpox) in Australia. Prior to the introduction of the vaccine, there were around five to eight deaths per year from this disease.
COVID also poses a bigger risk to children than influenza. During the 2009 H1N1 (swine flu) influenza pandemic, more than 1,000 children were hospitalised and 11 died.
It’s statistics like these that were behind the United States’ Centers for Disease Control and Prevention’s decision to recommend COVID vaccination for children.
CDC
How can we keep children safe?
Australia should follow the lead of countries that have already started to vaccinate children against COVID, such as the United States and Canada. However this is unlikely to happen until mid-to-late January next year.
This delay means public health measures will be vital to keep COVID under control in the community. As the experience of England has shown, high adult vaccination levels aren’t sufficient to protect children and prevent the virus from spreading in schools.
States that have planned to further ease restrictions should pause those plans until children have had the chance to be vaccinated.
We also need to do more to protect our schools. COVID is an airborne disease, meaning the virus drifts through the air like cigarette smoke. Masks and ventilation can help protect us, but ventilation involves much more than just opening a window.

Shutterstock
As the OzSAGE independent scientific advisory group explains, we need a comprehensive package of measures, including the use of HEPA air cleaners, to keep our schools safe.
Even after all of Australia’s children have had the chance to be vaccinated, we’ll need to keep some basic public health measures, such as improved ventilation, in place.
Read more:
COVID doesn’t need to run rampant. Here are 6 ways to keep cases low in the next year
COVID vaccines are very effective at preventing severe disease, but they’re not perfect and don’t completely prevent transmission. Their effectiveness may also diminish in the face of new variants of the virus.
As the sudden emergence of the Omicron variant has shown, the pandemic won’t end until global vaccination levels are much higher. Australia can do our bit by vaccinating as much of our population as possible, while also donating vaccines and manufacturing technology to developing countries in the region.
![]()
Dr Zoë Hyde is a member of the OzSAGE independent scientific advisory group.
– ref. We shouldn’t lift all COVID public health measures until kids are vaccinated. Here’s why – https://theconversation.com/we-shouldnt-lift-all-covid-public-health-measures-until-kids-are-vaccinated-heres-why-172625







