Source: The Conversation (Au and NZ) – By Dion O’Neale, Lecturer – Department of Physics, University of Auckland; Principal Investigator – Te Pūnaha Matatini, University of Auckland

Phil Walter/Getty Images
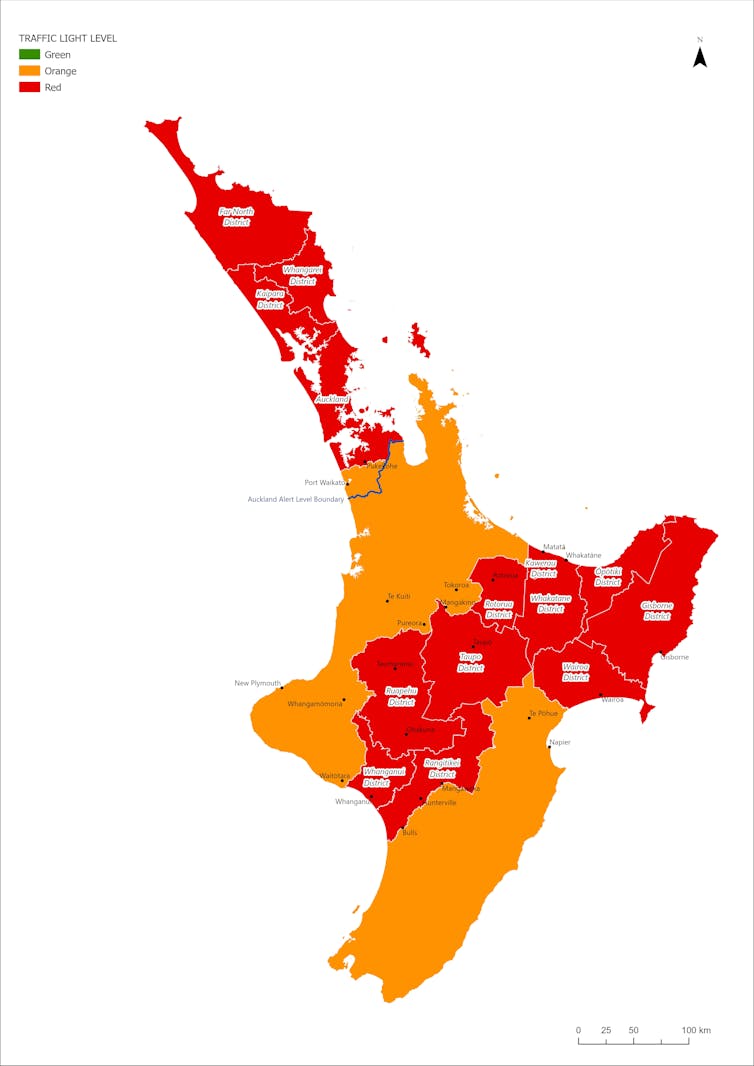
Despite the emergence of the new Omicron variant, New Zealand will move to a new COVID-19 Protection Framework this Friday, with a traffic light system to mark the level of freedoms for each region.
Auckland and other parts of the North Island that are battling active outbreaks or have low vaccination rates will start at red, which means hospitality and businesses will be largely open only for fully vaccinated people. The rest of the country will be in orange, which allows for larger gatherings but restricts access for those who remain unvaccinated.
From December 15, the Auckland boundary will lift and Aucklanders will be free to travel around the country, despite the ongoing community outbreak in which 23% of cases have been children under 12 and 14% were fully vaccinated.
Provided, CC BY-NC
To travel outside the Auckland boundary, anyone aged 12 or over will need to be fully vaccinated or have had a negative COVID-19 test within three days of departure. This will reduce the number of infected people leaving Auckland, but cases will spread across the country as people travel to see whānau and go on holidays.
As part of our research to build a population-based contagion network, we used electronic transaction data from previous years to derive movement patterns across the country. We show that during weeks without public holidays, just over 100,000 travellers left Auckland to visit one or more other regions.
For the summer period of 2019-2020, close to 200,000 people left Auckland each week, with travel peaking over the Christmas and New Year period. The most common destinations for these trips were Thames-Coromandel (30,000 people), Tauranga (17,000 people) and Northland (15,000 people).
Vaccination remains the best protection
While full (two-dose) vaccination levels in Auckland are almost at 90% — remembering that 90% of eligible people means only about 75% of the total population, with lower rates for Māori — rates are much lower in many places Aucklanders like to visit over summer. This provides much less protection, against both illness and transmission, and any outbreak would be larger and more rapid.
Vaccination coverage in these areas is increasing but is unlikely to be at 90% before Christmas. Holiday destinations also have health infrastructure designed for the much lower local population and face additional pressures if visitors get sick.
New Zealand’s outdoor summer lifestyle might be an advantage; transmission is greatly reduced outdoors with good air movement. But people should remain mindful anytime they move into an environment with less ventilation, such as using the toilet at the beach or sharing a car. A good rule of thumb is if you can smell perfume in the air then there’s a transmission risk.
COVID-19 is passed on through the air we breathe, which is why masking remains important, as long as the mask fits properly.
People planning to travel should reduce their risk of exposure during the two weeks before a trip.
-
Skip the office party (especially if they are held indoors)
-
consider postponing meetings until after the holidays rather than having them during the days before people are likely to travel around the country
-
if you decide to go ahead, make sure gatherings and parties are outdoors
-
avoid alcohol as it can increase the likelihood of risky behaviour
-
limit yourself to one meeting per week (if someone is infected, you’ll have a better chance to find out and self-isolate before passing it on)
-
use your contact tracer app, always
-
shop online
-
wear a mask anywhere there is a crowd, even outdoors.
Protecting people in regions with lower vaccination rates
Vaccination is the best step to reduce spread and symptom severity. But it’s not perfect. The risk of “breakthrough” infections depends on the intensity of exposure – short exposure to an infected person is less likely to result in infection and meeting indoors poses a higher risk.
When people are vaccinated, we’d expect to see most transmission happening in dwellings where people are together for long periods of time. For anyone with a breakthrough infection, vaccination approximately halves the chance of transmitting the virus.
Vaccination also reduces the risk of developing symptoms, and greatly reduces the risk of needing hospitalisation. But having milder symptoms can make it harder to detect cases, which means it remains important to get tested.
The most popular places New Zealanders like to visit over summer are remote and people living there haven’t had the same easy access to vaccination as those living in bigger cities.
Nearly a third of Northland’s eligible population remains unvaccinated, the East Cape is only 65% fully vaccinated and parts of the Coromandel Peninsula are also sitting well under ideal vaccination rates.
These places also have fewer testing facilities, which could mean outbreaks become harder to detect and manage. Many rural communities aren’t connected to town supply, so wastewater testing won’t be as useful, and emergency medical attention is harder to access.
Planning to manage COVID infections
Many residents in these remote towns, including iwi leaders, are asking holiday makers to stay away, regardless of vaccination status. Māori are already disproportionately represented in our COVID-19 statistics and have more young people who can’t be vaccinated yet.
By travelling to areas with low vaccination rates among the Māori population we risk compounding tragedy in places where health services would not cope with the level of illness.
Anyone choosing to go on holiday after weighing these factors should have a plan for what they’ll do if they or someone on their group develops COVID-like symptoms while away from their usual health support systems.
Questions to ask include:
-
Where will you go to get a test?
-
What will you do while you wait for test results?
-
Will it be possible for you to self-isolate while you wait for a test result?
-
Where is the closest medical centre? Do they operate after hours?
-
Is there an ambulance service and how far is the nearest hospital?
-
Is there good phone reception? If not, what will you do in a health emergency?
-
How would you manage an outbreak in your holiday accommodation?
Campers should take extra precautions by wearing masks in shared kitchens and bathrooms and using their own cleaning and hygiene products. They should keep good social distance wherever possible and minimise contact with people they don’t know.
Family gatherings will also bring together different generations, with elders who may be more vulnerable and younger people who are more mobile and more likely to be infected. A group of New Zealanders who experienced COVID-19 put together a management kit with a list of things anyone travelling will find useful.
We would like to acknowledge the contribution of Kylie Stewart, a member of the team at Te Pūnaha Matatini and the HRC-funded project Te Matatini o te Horapa — a population-based contagion network for Aotearoa New Zealand.
![]()
Dion O’Neale receives funding from the Health Research Council and the Department of Prime Minister and Cabinet to provide research and advice on the spread of COVID-19 in Aotearoa, including the equity impacts of contagion. He is a Principal Investigator in Te Pūnaha Matatini.
Andrew Sporle runs a research consultancy which receives funding from the Health Research Council, MBIE (via research projects at the Universities of Otago, Victoria and Auckland), The University of Auckland and Ministry of Social Development, Oranga Tamariki. He is a executive member of Te Mana Raraunga and the Virtual Health Information Network.
Emily Harvey receives funding from the Health Research Council and the Department of Prime Minister and Cabinet to provide research and advice on the spread of COVID-19 in Aotearoa, including the equity impacts of contagion. She is a Principal Investigator in Te Pūnaha Matatini, and Senior Researcher at ME Research.
Steven Turnbull receives funding from the Health Research Council and the Department of Prime Minister and Cabinet to provide research and advice on the spread of COVID-19 in Aotearoa, including the equity impacts of contagion. He is a Research Fellow in Te Pūnaha Matatini.
– ref. As Aucklanders anticipate holiday trips, Māori leaders ask people to stay away from regions with lower vaccination rates – https://theconversation.com/as-aucklanders-anticipate-holiday-trips-maori-leaders-ask-people-to-stay-away-from-regions-with-lower-vaccination-rates-172682







