Source: The Conversation (Au and NZ) – By Vanessa Bryant, Laboratory Head, Immunology Division, Walter and Eliza Hall Institute
The COVID vaccine rollout is underway in Australia, with people in phase 1b now eligible to be vaccinated.
So far, we have two vaccines available in Australia: the Pfizer/BioNTech vaccine, approved for people aged 16 and older, and the Oxford/AstraZeneca vaccine, approved for those over 18. Evidence has shown both vaccines are safe and offer near-complete protection against severe COVID-19, hospitalisation and, most importantly, COVID-related death.
Both vaccines are also safe and effective at generating immune responses in the elderly. But what about another vulnerable group — people with immunodeficiencies? Many people with immunodeficiencies are included in group 1b and will now be thinking about getting their vaccine.
Although we’re still gathering data to determine whether COVID vaccines will work as well in people with immunodeficiencies as they do in the general population, they’re likely to offer at least a reasonable degree of protection. And importantly, we know they’re safe.
What are immunodeficiencies?
Immunodeficiencies are conditions that weaken the body’s ability to fight infection. People’s immune system may be compromised for many reasons, and this can be transient or lifelong.Primary immunodeficiencies occur when some or all of a person’s immune system is missing, defective or ineffective. These are rare and often genetic diseases that may be diagnosed early in life, but can occur at any age.
Examples of primary immunodeficiencies include severe combined immunodeficiency (SCID) and common variable immunodeficiency (CVID).
Read more: What does it mean to be immunocompromised? And why does this increase your risk of coronavirus?
Secondary immunodeficiencies are acquired, and more common. They may occur as a result of other diseases (for example, via HIV infection), treatments and medications (such as chemotherapy or corticosteroids), or environmental exposure to toxins (for example, prolonged exposure to heavy metals or pesticides).
Sometimes the immune system in people with immunodeficiencies can react in exaggerated ways too, and cause autoimmune disease (such as rheumatoid arthritis or gut inflammation). So it sometimes makes more sense to describe the immune system as “dysregulated”, rather than “deficient”.
Immunodeficiencies, COVID-19 and vaccines
People with secondary immunodeficiencies are generally at higher risk of becoming infected with SARS-CoV-2 and of developing severe disease. Surprisingly, although people with primary immunodeficiency may be at greater risk of getting infections, including COVID, most are no more susceptible to developing severe COVID compared with the overall population.
This may be because the most severe COVID-19 symptoms are usually not due to gaps in immunity, but to an overactive immune response to SARS-CoV-2.
In fact, immune-suppressing steroids may be an effective treatment for severe COVID. Clinical trials looking into this are underway.
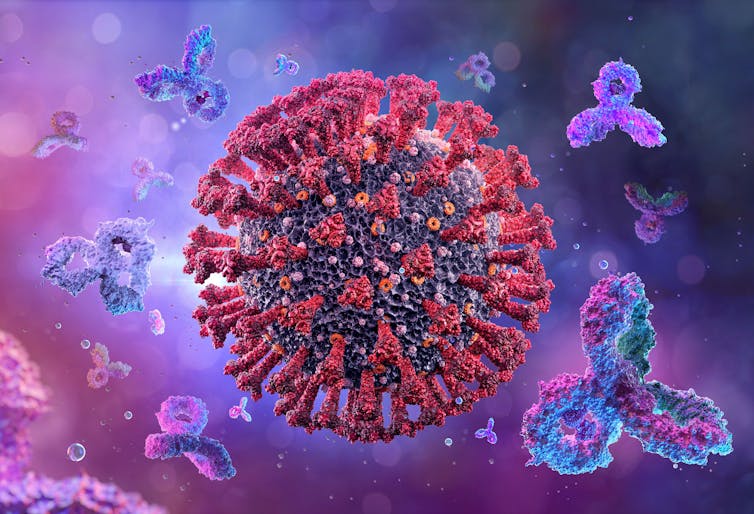
However, as vaccines work by mobilising our immune systems, for people who have a weaker immune system to begin with, vaccines may not be as effective. They may generate an incomplete or short-lived response, so people with immunodeficiencies may need additional boosters to maintain protective immunity.
Read more: What is a virus? How do they spread? How do they make us sick?
Efficacy and safety
It’s difficult to assess COVID vaccine efficacy in people with immunodeficiencies, because people with primary immunodeficiencies or cancer weren’t included in clinical trials.
A very small number of people with HIV have been included in trials of a few of the vaccines, but limited data is publicly available. So it’s too early to draw any firm conclusions on whether the vaccines will be as effective in people with HIV as for the general population.
We also don’t yet know how long immunity to COVID-19 or COVID vaccines lasts. This will be particularly important for immunodeficient people. Research is underway to determine whether they’ll need booster jabs more frequently to maintain immunity.

We do know the vaccines are safe for this group.
Neither the AstraZeneca nor the Pfizer vaccines can cause an infection, so they won’t present a problem for people with immunodeficiencies (or for elderly people, who may also have weakened immune responses).
Usually, we avoid giving “live attenuated” vaccines (vaccines that contain weakened elements of the virus) to anyone with immunodeficiency. Because of their weakened immune systems and increased susceptibility to infection, there’s a chance they could develop a full-blown infection. An example of this is the chickenpox vaccine. But no live attenuated COVID vaccines have been approved anywhere in the world.
Preliminary evidence from vaccine rollouts around the world has shown COVID vaccines are safe for immunocompromised people with cancer. Although, if you’re going through cancer treatment, you should discuss the timing of your vaccination with your specialist.
There have been no unusual safety concerns to indicate any increased risk for HIV-positive people receiving any of the COVID vaccines either.
Get the jab
Vaccination is most definitely recommended for people with immunodeficiencies, and they’re included in priority groups for vaccine rollout in Australia. Group 1b includes people with underlying medical conditions which may place them at higher risk from COVID-19, including “immunocompromising conditions”.
If you have a diagnosed immunodeficiency or autoimmune disease, you can talk to your doctor or specialist for specific advice on the timing of your COVID vaccination and your condition. There’s generally no reason to change your normal medications or therapies before receiving the vaccine.
Organisations including the Australian Society of Clinical Immunology and Allergy and the Immune Deficiency Foundation of Australia have published resources which offer guidance for people with immunodeficiencies in relation to COVID vaccination.
– ref. We don’t yet know how effective COVID vaccines are for people with immune deficiencies. But we know they’re safe — and worthwhile – https://theconversation.com/we-dont-yet-know-how-effective-covid-vaccines-are-for-people-with-immune-deficiencies-but-we-know-theyre-safe-and-worthwhile-155741







