Source: The Conversation (Au and NZ) – By Centaine Snoswell, Research Fellow Health Economics, The University of Queensland
The COVID-19 pandemic has resulted in rapid changes to the way Australians access health care. We’re now using telehealth more than ever.
Last week’s federal budget confirmed a six-month extension of Medicare subsidies for telehealth consultations, worth A$2.4 billion. It also included A$18.6 million for the preparation of permanent telehealth infrastructure beyond March 31 next year.
This goes some way to recognising telehealth is not only an important tool in our pandemic response — it’s much needed in our health system.
To fully realise the potential of telehealth, we need to recognise it’s more than just appointments via phone or videoconference.
COVID-19: a game changer for telehealth in Australia
In March, telehealth services were funded for all Australians under the Medicare Benefits Schedule (MBS).The package covered phone and videoconsultations with GPs, specialists, nurse practitioners and allied health professionals (like physiotherapists, social workers and psychologists). This complemented existing MBS funding for medical videoconsultations for people in rural communities.
We saw a rapid uptake — more than 35% of MBS-funded consultations were conducted via telehealth in April 2020.
Read more: Telehealth in lockdown meant 7 million fewer chances to transmit the coronavirus
There’s more to telehealth than phone calls and videoconferencing
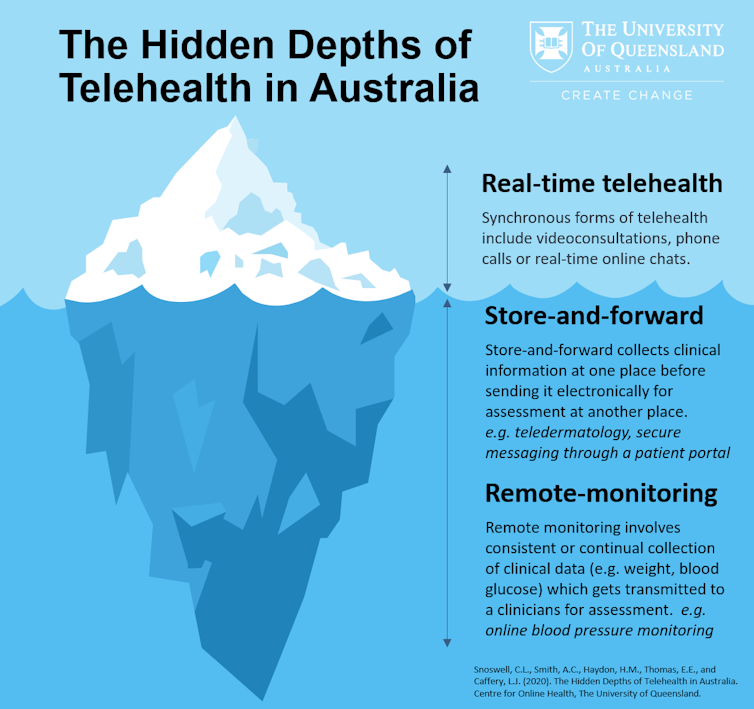
There are three main forms of telehealth: “real-time”, “store-and-forward” and “remote patient monitoring”.
Real-time is largely what we’ve got in place now — clinical consultations via phone and videoconferencing.
During the pandemic, health professionals have heavily favoured telephone over videoconsultations. More than 91% of MBS-funded telehealth services are delivered by phone.

While telephone can be effective in some situations (for example, history taking, triaging or referrals), videoconsultations can vastly improve the likelihood the clinician will make an accurate diagnosis.
Evidence shows videoconsultations can be as effective as in-person consultations, when it’s appropriate to use telehealth, regardless of the type of clinician.
Store-and-forward is the collection of clinical information and the process of sending it online.
A common example is when a patient or their GP photographs a skin lesion and sends the image to a dermatologist for an opinion and management advice.
Store-and-forward services exist in small silos in Australia. They often rely on hospital or commercial funding for support because they’re not currently funded on the MBS.
Store-and-forward services are offered around the world for a variety of conditions. Evidence shows they make services more accessible and cost-effective, and clinicians are generally satisfied with them.
Read more: What can you use a telehealth consult for and when should you physically visit your GP?
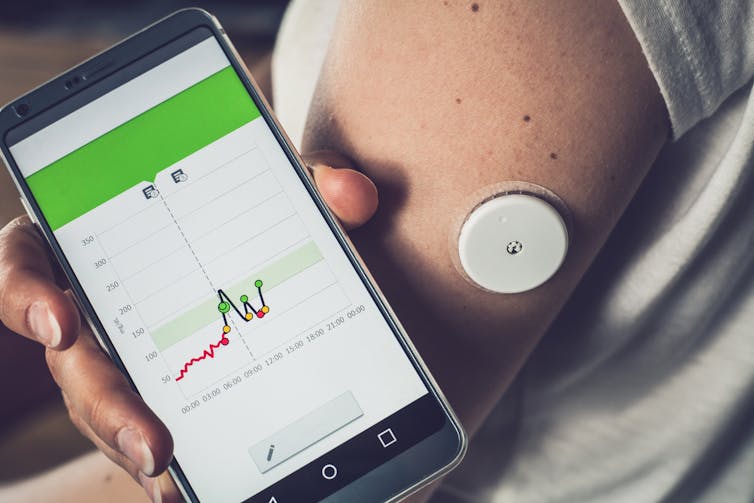
Remote patient monitoring, also called in-home monitoring or telemonitoring, involves collecting disease-specific health information and watching how it changes over time.
We can monitor conditions such as high blood pressure or diabetes (that often don’t have symptoms) using standard blood pressure machines or blood glucose monitoring devices that interact with apps or the internet.
If a patient’s readings fall outside healthy limits, an alert can be sent to both the patient and their primary care team.
Regular feedback combined with education and support can enable people to better self-manage their condition.
Remote monitoring is used internationally to manage chronic diseases, with good results. A recent review showed it led to positive outcomes in 77% of studies, with more people staying well and out of hospital for longer.
While there are a number of trials or small clinician-driven programs in Australia, lack of infrastructure and funding have prevented the wide roll-out of remote monitoring programs in the community.
Pleasingly, the federal budget has pledged money to begin working on infrastructure to monitor implantable devices, which will hopefully lead to interactive remote monitoring of patients with heart disease.
Choosing the right type
The choice of real-time, store-and-forward or remote patient monitoring should take into account the patient’s needs and their specific condition. It should also consider the cost of the service for the patient, provider and health system.
These lesser-used types of telehealth provide greater opportunity for multi-disciplinary care, and enable certain monitoring tasks to be redirected to nursing and allied health professionals, where appropriate.
For example, a nurse or pharmacist can review blood pressure readings and provide feedback to patients (and they can refer the patient for GP or specialist input if needed).
Remuneration for telehealth services should be commensurate with the amount of time, effort and skill required to provide the consultation. Incentivising video consultations (for example by subsidising them at a higher rate than telephone consultations) may be one way of encouraging clinicians to use them.
Thinking more broadly
Health systems around the world are not only battling the pandemic, but also the tsunami of chronic disease. So changes to the way we provide health care are inevitable.
In Australia, conditions like heart disease, stroke and diabetes lead to high rates of ill health and death.
We need strategies that inform patients about, and engage patients in, their own health care. We also need funding that supports services and health outcomes, rather than purely “fee for service” encounters.
Read more: Coronavirus has boosted telehealth care in mental health, so let’s keep it up
Store-and-forward and remote patient monitoring hold significant potential for enhancing the long-term management of chronic conditions, and ensuring easier access to specialist health services through a better connected health system.
We made the necessary changes to ensure health care was accessible during the pandemic. Now is the time to capitalise on this change to achieve true reform.
Crucially, we need to think about how we can make changes to the health-care system to take advantage of all forms of telehealth.
– ref. Video and phone consultations only scratch the surface of what telehealth has to offer – https://theconversation.com/video-and-phone-consultations-only-scratch-the-surface-of-what-telehealth-has-to-offer-146580




