Source: The Conversation (Au and NZ) – By Larisa Labzin, Research Fellow, Institute for Molecular Bioscience, The University of Queensland
Could we have some immunity to SARS-CoV-2, the virus that causes COVID-19, without ever having been exposed to it?
Some new studies found people who were never symptomatic, exposed to, or tested positive for COVID-19 have immune cells that can recognise and possibly kill virus-infected cells.
How is this possible? And what does it mean for our fight against COVID-19?
Many common colds are coronaviruses
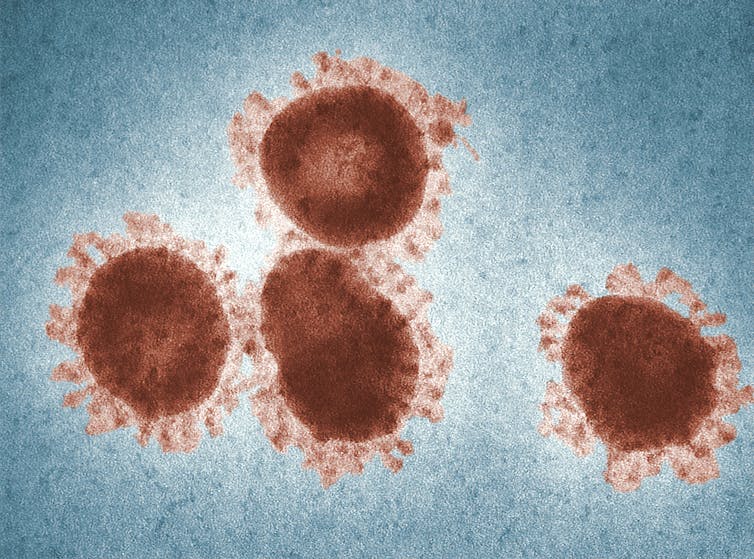
There are seven known coronaviruses that can infect humans. Three can cause severe respiratory symptoms: SARS-CoV-2, SARS-CoV-1 (which caused the 2002-04 SARS outbreak), and MERS-CoV (which was first identified in 2012).
The other four cause relatively mild colds, and are known as the common cold coronaviruses. It’s hard to find an exact figure, but one estimate suggests up to 30% of all common colds are caused by these coronaviruses, and up to 90% of us will have some antibodies against them in our blood. Like the other viruses that cause common colds (such as rhinoviruses), they show a strong seasonality, with a wave of coronavirus infections each winter.Immunity to these common cold coronaviruses is not very long–lasting, so we get re-infected with them all the time. We don’t know yet if our immunity to SARS-CoV-2 will also wane over time, and whether that means we could get re-infected.
Read more: Immunity to COVID-19 may not last. This threatens a vaccine and herd immunity
What did new studies find?
What these new studies did was expose some people’s blood to SARS-CoV-2. These blood samples were taken specifically from “healthy donors” – people who have never been confirmed to have coronavirus, or from whom blood was collected years before SARS-CoV-2 emerged.
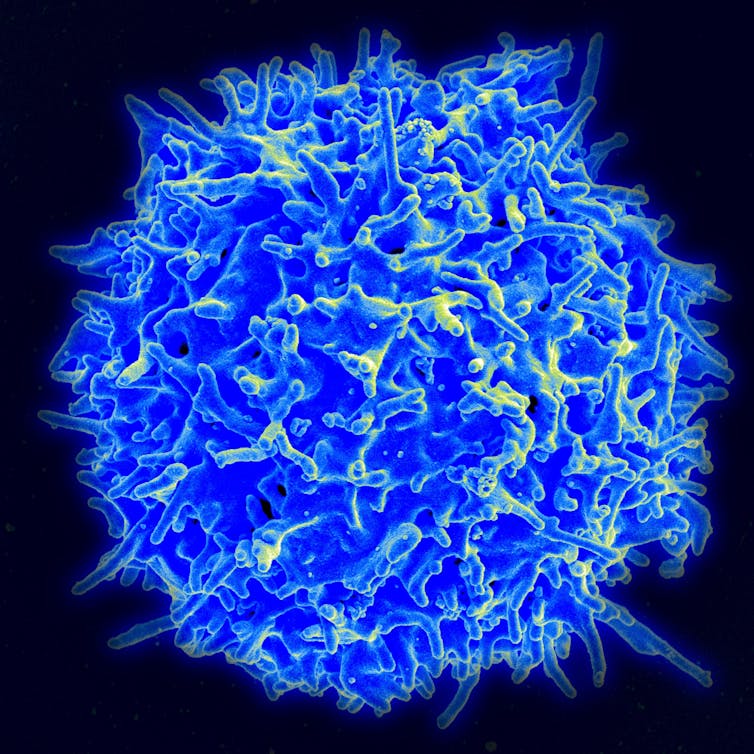
Depending on the study, between 20 and 50% of these people were found to have immune cells (called T cells) that could recognise SARS-CoV-2. This is unexpected, as usually specific T cells are only present after infection with the virus.
There are two possible explanations. Either those “healthy donors” were mildly infected with SARS-CoV-2 and didn’t show symptoms or develop antibodies, but they did develop a T cell response. Or, in the case of samples taken before the disease emerged, it means these T cells can recognise multiple coronaviruses, including common colds and SARS-CoV-2.
More than just antibodies
When we get infected with a virus like SARS-CoV-2, our immune system responds in a range of ways. It generates antibodies, which can neutralise the virus to stop it entering our cells. These antibodies are specific to the virus, and thus can be used to test whether we’ve had the virus before.
But besides antibodies, we have a host of other immune weapons in our arsenal for fighting off viruses.
T cells are specialised immune cells that have lots of functions (including helping us make antibodies) but are best known for being able to recognise and kill virus-infected cells. This is really important, because if the virus has evaded antibodies and managed to get into the cells, it can start replicating. Eliminating the infected cell is one of the most efficient ways to stop the infection.
Read more: Antibody tests: to get a grip on coronavirus, we need to know who’s already had it
T cells are master detectives
How do T cells know which of our body’s cells are infected with a virus? Because they can recognise small but specific snippets of viral proteins that our cells “present” on their surface. These viral snippets on the infected cell surface act like a beacon for the T cells to recognise and eliminate the virus-infected cells. Like antibodies, after the infection is cleared, we keep some of those T cells around in case we get reinfected with the same virus.
The small bits of virus presented on the infected cell’s surface can come from all parts of the virus, including the ones from inside the virus, which tend to be very similar across the different coronaviruses. That means a T cell that recognises a viral protein fragment from one type of coronavirus could potentially recognise the same fragment of viral protein that comes from a different coronavirus.
For example, if a virus was like a car, the antibody might recognise and bind to the outside, and it would only recognise a certain colour, year, and type of car.
But the T cell could recognise the specific bits, like the engine. So if the same engine was in loads of different cars, even though you might have really different cars, as long as it’s a petrol engine the T cell would recognise it. So it’s possible some of our T cells that were formed during a common cold infection are recognising SARS-CoV-2 and helping our immune system have a headstart for fighting SARS-CoV-2.
So these T cells can be cross protective — they work against different coronaviruses — and they can be very longlasting. In patients who recovered from SARS-CoV-1, specific T cells were still detectable up to 11 years later. This T cell memory could protect us from developing severe COVID-19, and could possibly explain why some people get so sick with COVID-19 while other people do not.
It’s not all rosy
While T cells represent another measure of whether people have been infected or not, we can’t use them as a quick diagnostic tool because detecting virus-specific T cells is far more slow, laborious and difficult than detecting antibodies.
We also don’t know yet what this pre-existing T cell immunity means for immune protection. We don’t even know whether the specific T cells generated during SARS-CoV-2 infection will be enough to protect us from COVID-19, and how important they are compared with the antibody responses.
Therefore, the most successful vaccines will likely induce both protective antibody and T cell responses to SARS-CoV-2.
Read more: Vaccine progress report: the projects bidding to win the race for a COVID-19 vaccine
– ref. Exposure to common colds might give some people a head start in fighting COVID-19 – https://theconversation.com/exposure-to-common-colds-might-give-some-people-a-head-start-in-fighting-covid-19-143455







