Source: The Conversation (Au and NZ) – By Stephen Carbone, Honorary, School for Population and Global Health, University of Melbourne
The battle against the mental health consequences of the coronavirus pandemic is just beginning. Governments and researchers are mapping how best to prevent the predicted rise in mental health issues we face in coming months and beyond.
This involves not only preventing a wave of mental disorders from starting but also preventing increased difficulties in people already living with poor mental health.
Read more: Can’t sleep and feeling anxious about coronavirus? You’re not alone
Is more outreach the answer, where mental health teams proactively go into the community to visit people in their homes?
Do we best focus on social policies and economic support to ease the financial and mental health pressure of job losses, isolation and increased stress?What other evidence-based ways of flattening the mental health curve are there? And once these services start, how do we make sure people actually use them?
Here’s what we face
People are already reporting psychological distress during the pandemic. And we’re just starting to collect Australian data. One preliminary study shows about 30% of survey participants have moderate to high levels of anxiety and depression. More Australian surveys are underway.
Without this urgently needed data, we cannot model the likely increase in mental health burden that lies ahead, and the impact various measures could have.
Flattening the mental health curve
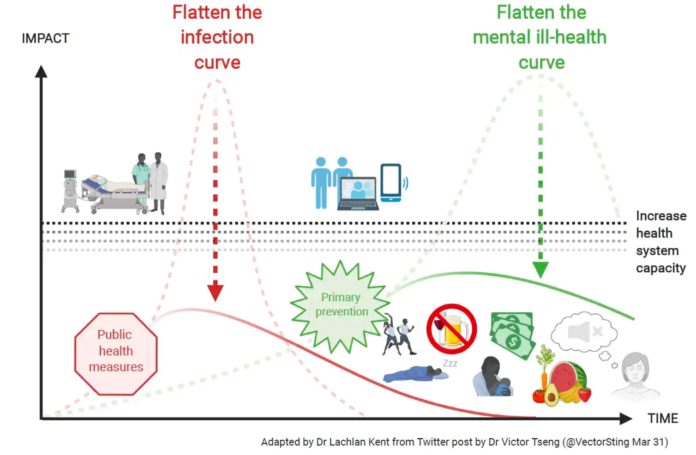
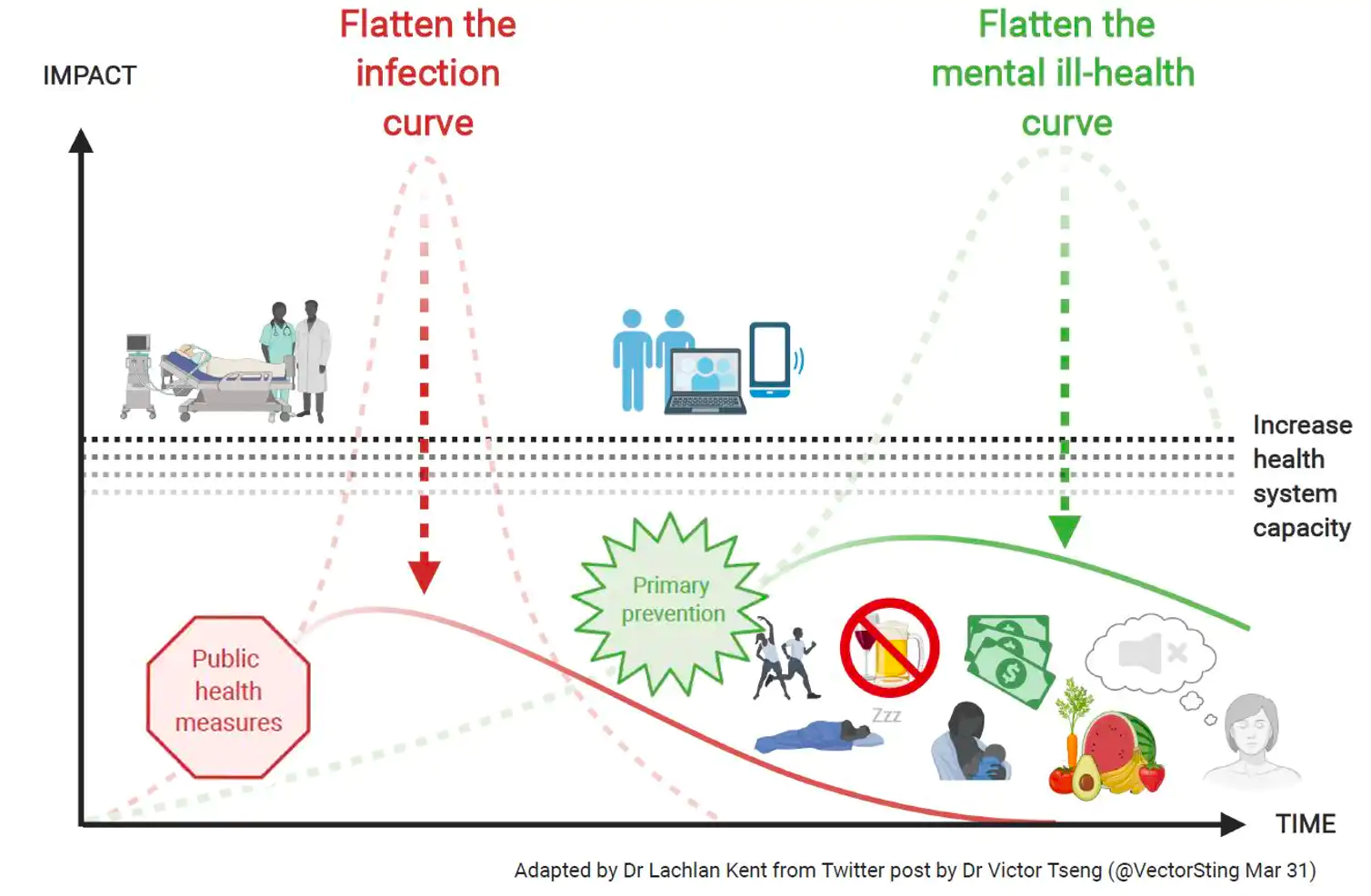
The “two-pronged” approach Australia is using to deal with the virus – preventing transmission and ramping up our health-care system to cope – also provides an excellent blueprint for managing the pandemic’s mental health impacts.
We need to focus on preventing new cases of mental disorders and we need to increase the capacity of our mental health-care system to manage any increase in people needing help.
The federal government has taken steps to increase the capacity of our mental health-care system.
These have included introducing Medicare items for telehealth mental health consultations, boosting existing phone and online support services for the public and frontline health workers, and extending access to some psychosocial support services for mental health clients in the community.
While these measures are vital, on their own they will not flatten the mental health curve. These services can help people recover once they have developed a mental disorder, but they do not prevent these conditions in the first place.
Some current policies are likely to help and need to continue
Federal government action to support people through the economic shocks of COVID-19 – including JobSeeker and JobKeeper payments, measures to reduce financial stress on mortgage holders and renters – will be crucial in flattening the mental health curve.
These policies must be kept in place for as long as possible if they are to prevent mental ill-health in the coming months and years. That’s because the links between unemployment or financial stress and mental health conditions are significant.
The government also needs to address some of the underlying issues that are key social determinants of mental health – to ensure equitable access to education, employment, and income and housing security – in the longer term (and beyond the current crisis).
This is vital if we are to address the higher rates of mental ill-health in less advantaged people.
We already have good evidence of the types of programs that prevent mental ill-health.
These programs can help counteract the impact of risk factors for mental ill-health that have escalated during the pandemic, such as social isolation, parenting stress, workplace stress, grief and loss, and family violence.
So the federal government should consider a second mental health funding package to scale them up.
Here’s what the evidence says helps prevent mental ill-health in two major groups.
Children, young people, their parents and carers
The mental well-being of children, young people, their parents and carers should be a priority. Some parents are struggling with the loss of work. Others are working from home and home-schooling their children. All are less able to access their usual social supports.
Certain parenting programs can reduce the chance of conduct disorder, depression and anxiety among children. Many of these are designed for online delivery.
For instance, one evidence-based program helps parents learn useful strategies that are particularly important now they are spending more time with their teens under trying circumstances.

Programs that provide practical and emotional support can help reduce the stress many parents are feeling. There is evidence programs involving nurses visiting parents with young children at home can lessen the risk of child maltreatment and therefore subsequent mental health issues.
We also have evidence-based programs to help children and young people acquire the social and emotional skills that contribute to resilience.
Most of these resilience programs are designed for schools but are often poorly implemented due to the lack of time, resourcing and professional development to support schools and educators to deliver them.
So we need additional resources for schools and professional development for educators to better implement them.
Adults and older Australians
Adults also need strategies to promote their mental well-being, including self-care, and knowing when and how to ask for help.
As we are seeing, demand for mental health services in Australia has decreased and not increased, as expected, during the pandemic. This may reflect health concerns or difficulties people have accessing the right services. So we need to design service models that are safe and fit-for-purpose in the current climate.
Preventing work-related mental-health conditions is also important. This needs employers and employees to collaborate to reduce the chance of these conditions developing.
So evidence-based prevention programs are more relevant than ever as employers and employees confront new stressors, including changes in work practices caused by COVID-19.
People on the frontline of pandemic response efforts, such as health-care workers, should be a key target for prevention programs given the high levels of stress many have experienced.
Tackling loneliness is also vital and the elderly should be a prime focus.
The federal government has increased funding for the community visitors scheme, when volunteers visit older people to provide friendship and companionship, which is an excellent start.
Befriending initiatives could also work for other socially isolated people.
Where to next?
COVID-19 has disrupted our lives and our livelihoods, and the wide-ranging personal, social and economic impacts of this pandemic will continue to be felt for many months and years.
We already have a number of evidence-based approaches to prevent common mental health conditions and that can be scaled up immediately. We also need to support research to find new and more effective approaches.
But parallel efforts to encourage people to seek help if they are experiencing a mental health condition, and ensuring they get the right help, are also crucial.
This pandemic highlights the importance of innovation and trying to provide services in new and more accessible ways – whether through better use of digital mental health programs, telehealth consultations or outreach services – to ensure people can still access mental health supports and services how and when they need them during these difficult times.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
– ref. We need to flatten the ‘other’ coronavirus curve, our looming mental health crisis – https://theconversation.com/we-need-to-flatten-the-other-coronavirus-curve-our-looming-mental-health-crisis-137170