Source: The Conversation (Au and NZ) – By Sarah Versitano, Academic, Master of Art Therapy Program, Western Sydney University

Creating art for healing purposes dates back tens of thousands of years, to the practices of First Nations people around the world. Art therapy uses creative processes, primarily visual art such as painting, drawing or sculpture, with a view to improving physical health and emotional wellbeing.
When people face significant physical or mental ill-health, it can be challenging to put their experiences into words. Art therapists support people to explore and process overwhelming thoughts, feelings and experiences through a reflective art-making process. This is distinct from art classes, which often focus on technical aspects of the artwork, or the aesthetics of the final product.
Art therapy can be used to support treatment for a wide range of physical and mental health conditions. It has been linked to benefits including improved self-awareness, social connection and emotional regulation, while lowering levels of distress, anxiety and even pain scores.
In a study published this week in the Journal of Mental Health, we found art therapy was associated with positive outcomes for children and adolescents in a hospital-based mental health unit.
An option for those who can’t find the words
While a person’s engagement in talk therapies may sometimes be affected by the nature of their illness, verbal reflection is optional in art therapy.
Where possible, after finishing an artwork, a person can explore the meaning of their work with the art therapist, translating unspoken symbolic material into verbal reflection.
However, as the talking component is less central to the therapeutic process, art therapy is an accessible option for people who may not be able to find the words to describe their experiences.
Read more:
Creative arts therapies can help people with dementia socialise and express their grief
Art therapy has supported improved mental health outcomes for people who have experienced trauma, people with eating disorders, schizophrenia and dementia, as well as children with autism.
Art therapy has also been linked to improved outcomes for people with a range of physical health conditions. These include lower levels of anxiety, depression and fatigue among people with cancer, enhanced psychological stability for patients with heart disease, and improved social connection among people who have experienced a traumatic brain injury.
Art therapy has been associated with improved mood and anxiety levels for patients in hospital, and lower pain, tiredness and depression among palliative care patients.

mojo cp/Shutterstock
Our research
Mental ill-health, including among children and young people, presents a major challenge for our society. While most care takes place in the community, a small proportion of young people require care in hospital to ensure their safety.
In this environment, practices that place even greater restriction, such as seclusion or physical restraint, may be used briefly as a last resort to ensure immediate physical safety. However, these “restrictive practices” are associated with negative effects such as post-traumatic stress for patients and health professionals.
Worryingly, staff report a lack of alternatives to keep patients safe. However, the elimination of restrictive practices is a major aim of mental health services in Australia and internationally.
Read more:
‘An arts engagement that’s changed their life’: the magic of arts and health
Our research looked at more than six years of data from a child and adolescent mental health hospital ward in Australia. We sought to determine whether there was a reduction in restrictive practices during the periods when art therapy was offered on the unit, compared to times when it was absent.
We found a clear association between the provision of art therapy and reduced frequency of seclusion, physical restraint and injection of sedatives on the unit.
We don’t know the precise reason for this. However, art therapy may have lessened levels of severe distress among patients, thereby reducing the risk they would harm themselves or others, and the likelihood of staff using restrictive practices to prevent this.
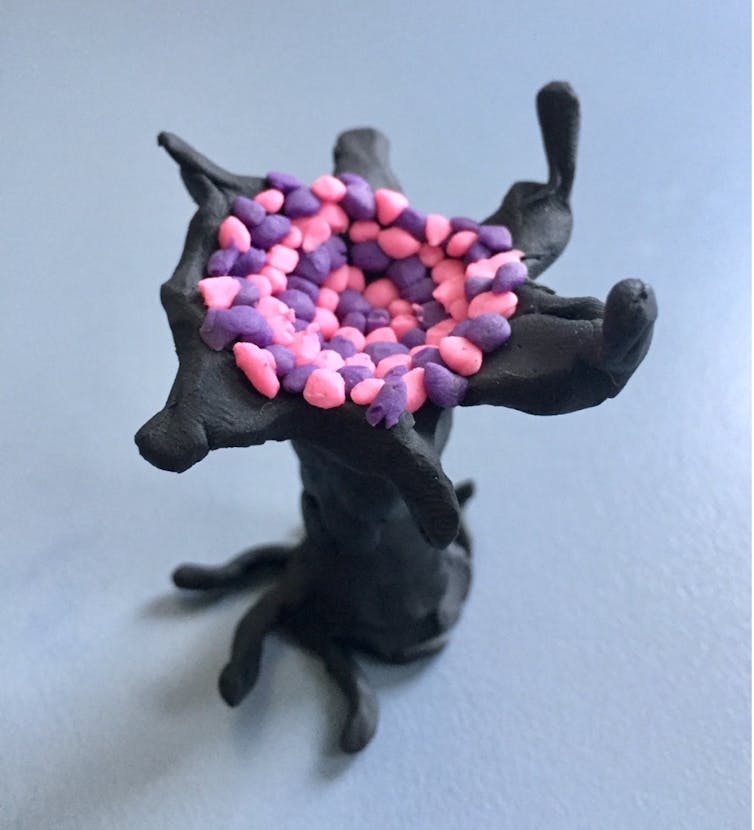
Author provided
That said, hospital admission involves multiple therapeutic interventions including talk-based therapies and medications. Confirming the effect of a therapeutic intervention requires controlled clinical trials where people are randomly assigned one treatment or another.
Although ours was an observational study, randomised controlled trials support the benefits of art therapy in youth mental health services. For instance, a 2011 hospital-based study showed reduced symptoms of post-traumatic stress disorder among adolescents randomised to trauma-focussed art therapy compared to a “control” arts and crafts group.

Author provided
What do young people think?
In previous research we found art therapy was considered by adolescents in hospital-based mental health care to be the most helpful group therapy intervention compared to other talk-based therapy groups and creative activities.
In research not yet published, we’re speaking with young people to better understand their experiences of art therapy, and why it might reduce distress. One young person accessing art therapy in an acute mental health service shared:
[Art therapy] is a way of sort of letting out your emotions in a way that doesn’t involve being judged […] It let me release a lot of stuff that was bottling up and stuff that I couldn’t explain through words.
A promising area
The burgeoning research showing the benefits of art therapy for both physical and especially mental health highlights the value of creative and innovative approaches to treatment in health care.
There are opportunities to expand art therapy services in a range of health-care settings. Doing so would enable greater access to art therapy for people with a variety of physical and mental health conditions.
![]()
Sarah Versitano is a PhD Candidate at Western Sydney University and works for the Sydney Children’s Hospitals Network, which is part of NSW Health. She has received funding from the Health Education and Training Institute (HETI) for the Mental Health Research Award. She is a Registered Art Therapist with the Australia, New Zealand and Asian Creative Arts Therapies Association (ANZACATA) and Registered Clinical Counsellor with the Psychotherapists and Counsellors Federation of Australia (PACFA). She has delivered art therapy and psychotherapy in public and private hospital settings.
Iain Perkes works for the University of New South Wales and the Sydney Children’s Hospitals Network which is part of NSW Health. He has previously worked for numerous health services throughout NSW Health. He has received funding or awards from the Australian National Health and Medical Research Council (NHMRC), the International Association of Child and Adolescent and Allied Professions, (IACAPAP), the World Psychiatric Association (WPA), the Tourette’s Association of America (TAA), Tourette Syndrome Association (TSA), the NSW Institute of Psychiatry, The University of Sydney, and the Sydney Partnership for Health, Education, Research and Enterprise (SPHERE). He is affiliated with Neuroscience Research Australia (NeuRA) and the Health Education and Training Institute (HETI, NSW Health).
– ref. Lost for words? Research shows art therapy brings benefits for mental health – https://theconversation.com/lost-for-words-research-shows-art-therapy-brings-benefits-for-mental-health-221309



