Source: The Conversation (Au and NZ) – By Kate Manlik, Casual Academic and PhD Candidate, Macquarie University

ABC
The recent ABC mini-series, In Our Blood, offers a fictionalised account of Australia’s response to AIDS, focusing on the development of a partnership between impacted communities, health professionals and government.
Lesbians are placed at the centre of this narrative, but more needs to be done to ensure these representations capture the complex histories of AIDS information activism in Australia.
The series features two lesbian characters: activist Deb (Jada Alberts) and high-school teacher Mish (Anna McGahan). Deb and Mish are shown attending activist rallies, speaking up in meetings with government representatives, transforming their home into an office for AIDS activists, and caring for people living with HIV.
Their inclusion serves to historicise lesbians’ immense contribution to Australian AIDS activist movements – but it perpetuates a well-established trope of the “altruistic” lesbian carer and advocate.
In this re-telling, we risk forgetting that lesbians also protested their own exclusion from epidemiological, medical and public health information about AIDS.
Are lesbians at risk of HIV?
The answer is complicated.
While sex between cisgender women is thought to be low risk, several studies suggest that transmission is possible.
It is, however, important to understand how HIV risk transmission hierarchies can render lesbian and queer women invisible in our surveillance data.
When a person is diagnosed with HIV, risk transmission hierarchies are used to record their most probable source of exposure to the virus. In Australia, these risk hierarchies have never recognised female-to-female sex as a potential route for HIV transmission.
This means, for example, that if a woman reports having sex with both men and women, her exposure to the virus is recorded as “heterosexual contact”. If she has never had sex with a man but uses injecting drugs, her exposure is recorded as “injecting drug use”. And if she has never had sex with a man or used injecting drugs, her exposure is recorded as “undetermined”.
Yet, even if we understand sex between cisgender women as low risk, lesbians are not a homogenous group. Some lesbians use injecting drugs, have sex with men or could become infected with HIV through another source of transmission.
But for these lesbians to be included in HIV surveillance data, their sexual identities must be obscured.
Because of this, we have no way of knowing how many lesbian and queer women are living with HIV or have died from AIDS-related illness in Australia. Although, anecdotally, we do know that four of the first seven women diagnosed with HIV were lesbians.
ACON
Untold histories of lesbian AIDS activism
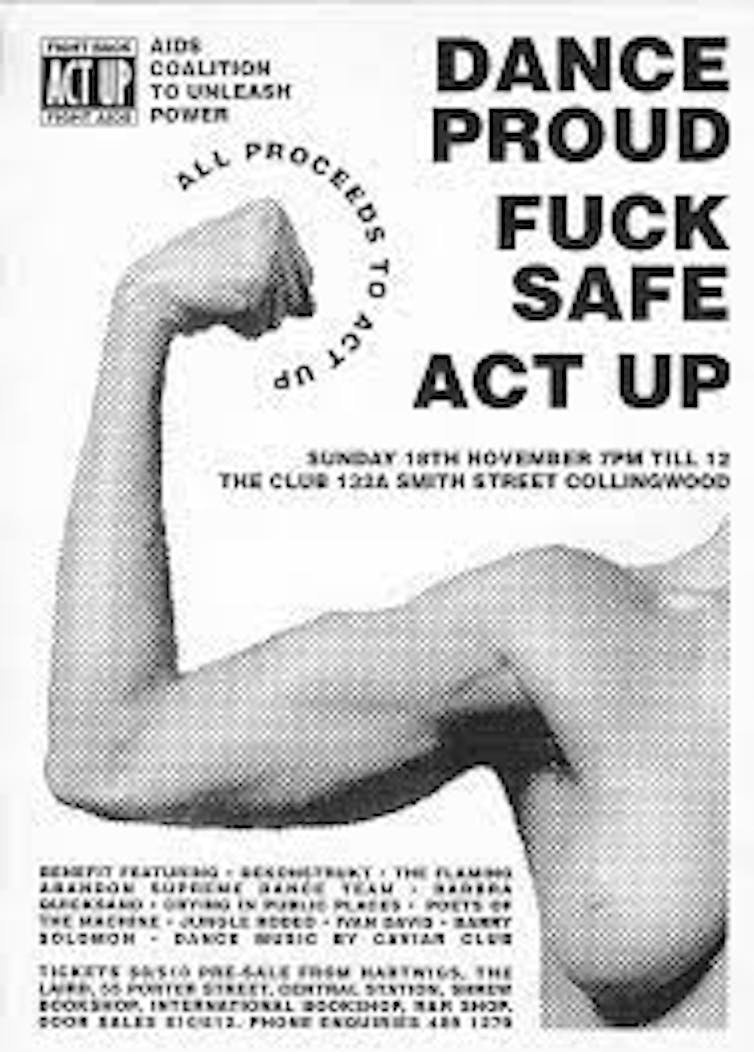
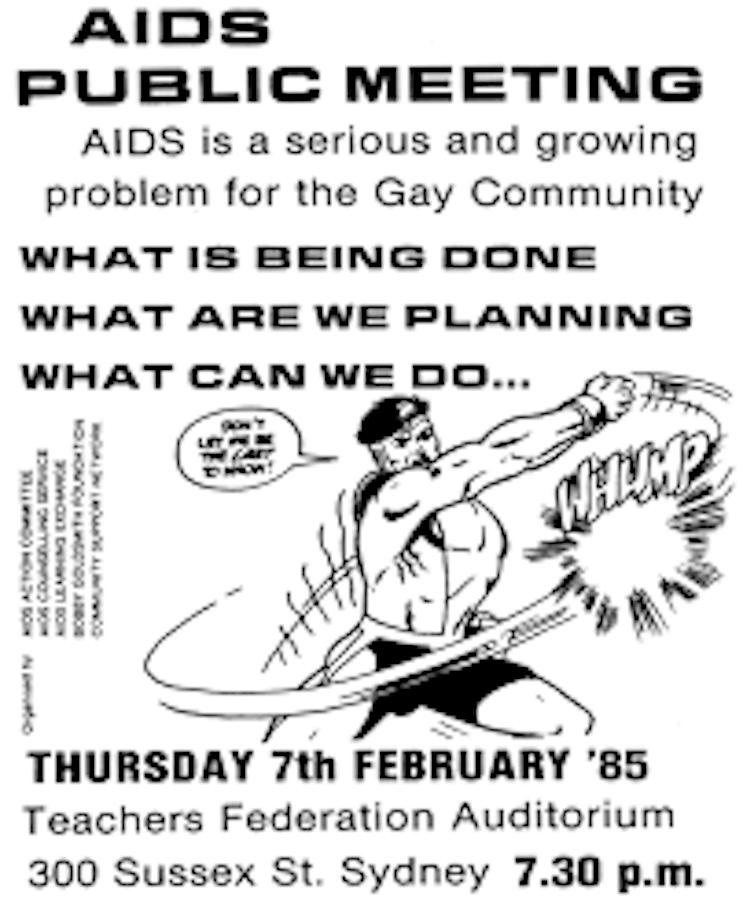
Since the 1980s, when In Our Blood takes place, lesbians have advocated for their inclusion in Australia’s public health, medical and epidemiological response to AIDS.
Much lesbian AIDS activism occurred from within Australian AIDS organisations, such as the AIDS Council of New South Wales (now known as ACON). In 1988, ACON’s Women and AIDS Working Group produced the organisation’s first lesbian information pack, entitled Sapph Sex – its title a pun on safe and sapphic sex.
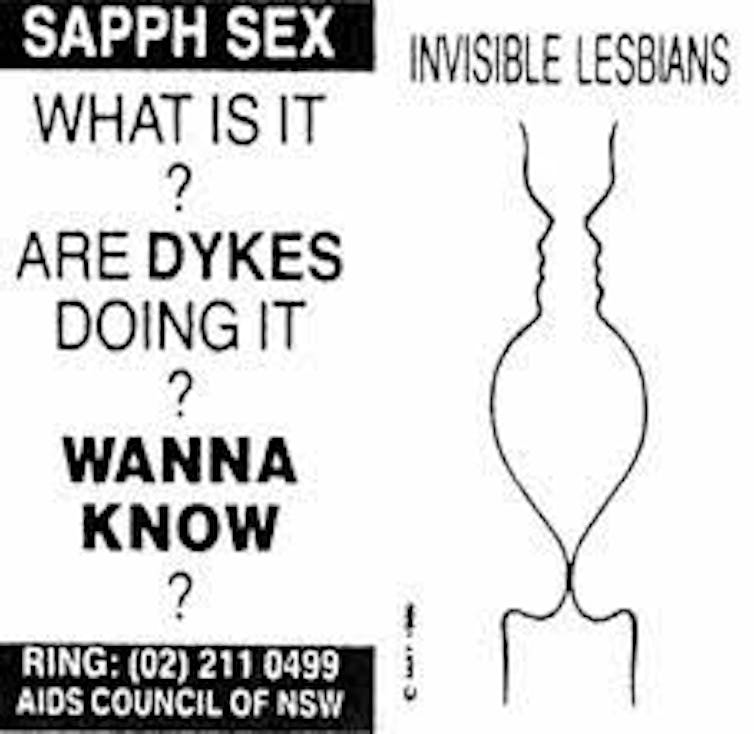
ACON
Outside the context of Australian AIDS organisations, activists used lesbian magazines to produce, debate and circulate lesbian-specific information about HIV. Lesbian magazines published articles contesting the dominant assumption that lesbians were “immune” to HIV, and provided a platform for HIV-positive lesbians to write on their experiences.
Readers of Australia’s largest lesbian magazine, Lesbians on the Loose, were also encouraged to write in to the magazine’s resident doctor, Doctor on the Loose, to request guidance on a range of health-related concerns.
During the height of the epidemic, Doctor on the Loose provided readers with advice on the risks associated with specific practices: sex, injecting drug use, sperm donation, and blood sharing rituals. In their responses, Doctor on the Loose worked to dispel common misunderstandings about HIV transmission:
you can’t catch it from toilet seats, sharing food, sharing joints, shaking hands or kissing (there is no evidence that tongue kissing passes on HIV).
HIV-positive lesbians were, of course, at the forefront of these activist endeavours. One such lesbian was Jennifer Websdale. As one of the first seven women diagnosed with HIV in Australia, she was committed to ensuring lesbians were visible as a distinct population in the global AIDS epidemic.
In 1991, Websdale received funding to attend the Ninth National AIDS/HIV Forum in New Orleans. When she returned to Australia, she coined the term “cuntaphobia” to describe the complex intersections of sexism and homophobia that work to silence HIV-positive lesbians in wider conversations about HIV.
ACON
Websdale died from AIDS-related illness in 1994 at the age of 33. Three decades on, her activism retains an enduring relevance.
As we move toward ending HIV in Australia, it is imperative for us to interrogate how our ingrained re-tellings of the Australian AIDS epidemic foreground some histories, and marginalise others.
After all, the project of ending HIV will require us to ensure that HIV prevention, testing and treatment information and services are available to all Australians – including lesbian and queer women.
![]()
Kate Manlik received funding from a Research Training Program (RTP) Scholarship while undertaking this research.
– ref. The ABC’s In Our Blood shines a light on lesbian activism during the AIDS crisis – but there’s more to their story – https://theconversation.com/the-abcs-in-our-blood-shines-a-light-on-lesbian-activism-during-the-aids-crisis-but-theres-more-to-their-story-202354




