Source: The Conversation (Au and NZ) – By Peter Breadon, Program Director, Health and Aged Care, Grattan Institute

New federal Health Minister Mark Butler says primary care is “in worse shape than it’s been in the entire Medicare era” and has made it his top health priority.
Primary care is any first point of contact with the health system, such as a GP clinic, dentist, or community pharmacy, but the government is likely to focus on GP clinics.
A new taskforce will advise the minister on how to spend A$750 million to improve access, chronic disease management, and affordability. The taskforce has until Christmas to come up with a plan, which is a big ask given where the system is now.
Taking lessons from what’s worked overseas, we’ve identified five key lessons about how Australia should reform general practice funding.
But first, let’s consider what’s gone wrong.
Primary care isn’t set up for the problems of today
Almost half of Australians have a chronic disease, such as heart disease, diabetes, asthma or depression. More than half of Australians over 65 have two or more. Those proportions have been rising fast in recent decades.
To help patients manage these conditions, GPs need ongoing relationships with patients (known as continuity of care), and a team working with them by providing routine care, outreach, coaching, and advice. That lets GPs spend more of their time working with the most complex patients, resulting in better care and outcomes.
But the way GPs are funded – and the way the primary care system is managed – makes this nearly impossible. GPs tell us they aren’t respected, are stressed out, and are set up to fail by a system that is fragmented, rigid, and unsupportive.
After decades of neglect, there are many problems to fix. Clinics often don’t have the right mix of staff, collaborating with specialists and hospitals is difficult, data systems are fragmented, and there are parts of Australia with poor access to care.
Read more:
Labor’s health package won’t ‘strengthen’ Medicare unless it includes these 3 things
One issue the taskforce must consider is how GP clinics are funded. While a simple boost to fees might be welcomed by practices, it can’t deliver the better access, quality, and affordability that Labor has promised. Australia’s approach has outlived it’s used-by date.
Here’s what Australia can learn from other countries that have transformed primary care funding:
1: Blend payments to strike the right balance
Australia is one of a small and shrinking list of countries that still mostly uses fee-for-service funding. There are payments to make care plans, and for working to improve quality measures (such as measuring risk factors or increasing immunisation rates), but the vast bulk still goes on individual GP consultations.
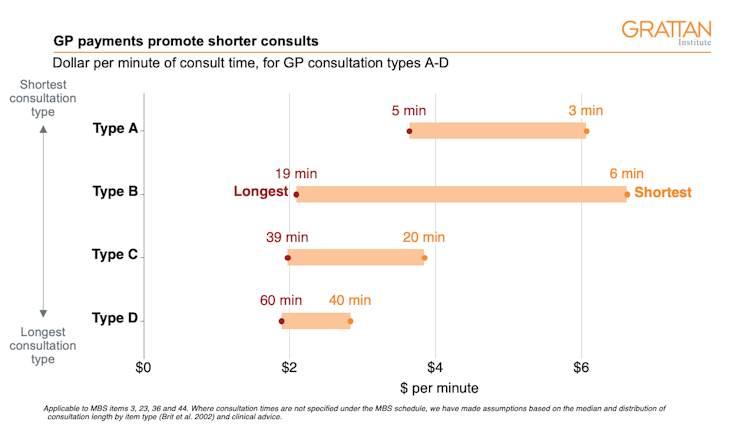
Shorter visits pay more, promoting a focus on speed not need – a poor fit for helping patients with complex needs.
Grattan Institute
Since the 1990s, many other countries have moved towards a “blended” funding model. After a patient enrols with with a particular doctor or clinic, GPs have ongoing responsibility for their patients and get flexible annual budgets for their care, along with a small fee for each visit.
This supports continuity of care and gives flexibility to provide different types of services, while keeping an incentive for GP consultations. It strikes a good balance between GP visits and other kinds of care, such as check-ins with a practice nurse, medication reviews from a practice pharmacist, or even support that goes beyond health care, such as help with housing or community services.

2: Adjust funding for health and social needs
Australia’s core primary care funding system, the Medicare Benefits Schedule, does little to match funding with a patient’s needs. As shown above, it promotes short consultations, no matter how complex the patient’s health needs. It largely ignores disadvantage, even though people who are poor are likely to be sicker.
Read more:
Poor and elderly Australians let down by ailing primary health system
New Zealand and Ontario (a province in Canada) introduced blended payments in the 1990s. However, they didn’t adjust annual patient budgets for clinical complexity or social need. Clinics received the same funding for treating someone who was healthy and wealthy as someone who was sick and poor.
It worked for practices in well-off areas, but not for those serving poorer communities, resulting in reduced services.
The mismatch of care and need is a big problem in all health systems. Blended funding must be adjusted to level the playing field, otherwise it could make that mismatch even worse.
3. Fund a multi-disciplinary team
The patient budget described above gives clinics flexibility to fund different types of workers, such as mental health nurses, community health workers, or pharmacists. But experience overseas shows this isn’t enough to bring about best-practice multidisciplinary teams.
The United Kingdom and New Zealand also provide direct funding for different kinds of workers. In the UK, the full cost is covered for 13 types of workers, ranging from paramedics and podiatrists to “link workers”, a new role that coaches patients to achieve their health goals, and connects them to social support and community activities.

Unsplash/Hush Naidoo Jade Photography
4: Step in when the market fails
In parts of rural Australia, even the best blended funding model won’t attract GPs. In some cases, the demand from patients is too low or unpredictable to make it worthwhile running a stand-alone clinic.
In these cases of market failure, a different model is needed. Federal and state governments should work together to jointly employ salaried GPs and other primary care staff, giving them roles that might span the primary care clinic and a local hospital.
As the National Rural Health Alliance proposed, this could take the form of non-profit, community-controlled organisations, with similarities to Aboriginal-controlled clinics and community health providers.
5: Recognise that change is hard and will take time
A new funding model will require different workforce roles, reporting and data. Experience shows clinics must have strong support to help them change.
An evaluation of the last major national attempt at primary care reform, Health Care Homes, recommended a change-management team within each practice with adequate training and protected time, as well as skilled external facilitators. In line with assessments in the UK, the evaluation also found that developing trust and peer support was crucial.
All this points to a staged roll-out over several years, with strong support within clinics, between clinics, and from Primary Health Networks, the regional bodies responsible for improving the primary care system.
A long-term plan for change is more complex than a tweak to the Medicare Benefits Schedule. But it will be vital to give a sector under strain enough support to adapt to a funding system that’s better for workers and patients alike.
Read more:
More visits to the doctor doesn’t mean better care – it’s time for a Medicare shake-up
![]()
Peter Breadon does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
– ref. General practices are struggling. Here are 5 lessons from overseas to reform the funding system – https://theconversation.com/general-practices-are-struggling-here-are-5-lessons-from-overseas-to-reform-the-funding-system-188902




