Source: The Conversation (Au and NZ) – By Angela Brown, Midwifery Program Director , University of South Australia

So far, there have been 57 confirmed and probable cases of monkeypox reported by Australian authorities.
In July, the Australian government issued a health alert for monkeypox as a communicable disease following the World Health Organization’s declaration of it as a public health emergency.
The disease has been reported at higher rates among men who have sex with other men. But this does not mean it can’t be spread to anyone. In fact, it has been seen in pregnant and birthing women and their newborn babies in some Western countries.
What do we know about monkeypox?
Monkeypox is a viral disease spread between animals and people.
The UK government guidance described the first case of “Monkey Pox” in 1958, when it was found in monkeys used for research purposes.
It was 1970 when it was first reported in human populations in the African country, Democratic Republic of the Congo. The disease is now endemic in some African countries including Nigeria, Liberia, Sierra Leone and the Democratic Republic of the Congo.
What does this mean for pregnant women?
Fortunately, monkeypox does not spread easily. The infection is spread by close physical contact, and so far there is limited information available about the impact on pregnancy, particularly in high income countries.
The virus can enter the body via broken skin, the respiratory tract or mucous membranes (the moist inner lining of cavities and some organs in the body).
The US Centers for Disease Control and Prevention advises the virus can be transmitted to a baby before birth via the placenta, and after the baby is born by close physical contact.
It also recommends pregnant, postnatal and breastfeeding women should be prioritised for medical treatment as there is a significant risk to the baby.
The Australian government’s treatment guidelines identify pregnant and breastfeeding women at high risk of severe disease from monkeypox infection. They also identify these groups as eligible for treatment and encourage health care providers to consult infectious disease specialists.
What symptoms should you watch for?
Symptoms of monkeypox can include headaches and fever, muscle and joint pain, tiredness, swollen lymph glands and a telltale rash with lesions that develop anywhere on the body.
The lesions change and will eventually burst, scab over and heal. The amount and location of the lesions can vary from lots all over the body to only a few that are isolated to one or two areas.
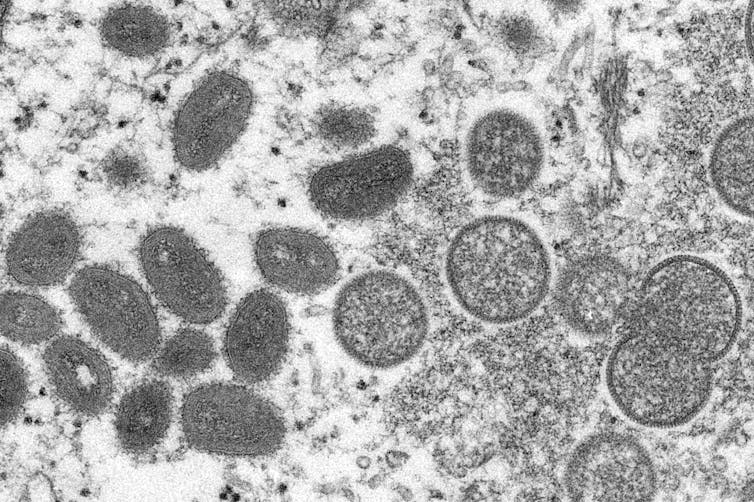
Cynthia S. Goldsmith, Russell Regner/CDC via AP
Read more:
Monkeypox in Australia: should you be worried? And who can get the vaccine?
Deadly for some
The European Centre for Disease Prevention and Control has said most people (who are not pregnant) have mild disease with recovery within a few weeks, but that the Nigerian cases have had a fatality rate of roughly 3%. Mortality is likely higher in vulnerable groups such as newborn babies and pregnant or breastfeeding women.
A recent paper published in medical journal The Lancet provides guidelines for doctors and midwives on the management of monkeypox infection during pregnancy. These guidelines include increased fetal monitoring and increased surveillance of the mother in hospital isolation rooms if necessary, depending on her symptoms.
If the woman has genital lesions at the time of birth, she may be offered a caesarean. The newborn baby will need careful monitoring and precautions to reduce the risk of transmission from the mother. Consultation with a specialist infectious diseases paediatrician is recommended in these cases.
The Australian government has supplies of a monkeypox vaccine called Jynneos, and this may be considered in cases in which a woman has had close physical contact with an infected person or meets other criteria. The safety profile of this medication in pregnancy is unknown, but it is thought to be able to be used following a risk and benefit analysis by the medical practitioner. Women should not seek vaccination without risk factors being present.
Read more:
Australia secures 450,000 new monkeypox vaccines. What are they and who can have them?
Known cases
Several cases of monkeypox infection were reported in the Democratic Republic of the Congo as a part of a larger study. The study wasn’t specifically looking at pregnant women, but four women were found to be pregnant in the study of more than 200 people with monkeypox infection.
Of the four women with monkeypox infection in pregnancy, two experienced miscarriage, one gave birth to a stillborn baby, and one gave birth to a living full-term baby. The three women who had fetal losses all experienced moderate to severe disease and lost their babies either in the first or second trimester of pregnancy.
Australian women shouldn’t be overly concerned at this stage given the low numbers of infected people in Australia. Women are highly unlikely to catch monkeypox unless they have had close contact with someone already infected with the disease or they have visited countries where the disease is endemic.
There are no known cases of women infected in pregnancy within Australia to date but there are such cases in the UK and US.
Avoiding contact with infected people and seeking early medical care if exposure is suspected is the best strategy as we watch the monkeypox situation evolve. Women can also monitor monkeypox advice from Australian authorities and speak with their midwife or obstetrician if they have any concerns.
![]()
Angela Brown does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
– ref. Monkeypox can be transmitted to babies during and after pregnancy. We should be watchful but not alarmed – https://theconversation.com/monkeypox-can-be-transmitted-to-babies-during-and-after-pregnancy-we-should-be-watchful-but-not-alarmed-188283








