Source: The Conversation (Au and NZ) – By Greg Kelly, Senior lecturer, The University of Queensland

Doctors and health experts have expressed shock on social media recently about the number of ICU patients on ECMO treatment, especially in Victoria.
ECMO, which stands for extra corporeal membrane oxygenation, is the life support of last resort for patients with severe heart and lung failure.
At any one time, a busy ECMO hospital would normally have three to five patients supported with ECMO. The number of patients on ECMO at the Alfred Hospital in Melbourne is hovering around 20, almost all because of COVID. In the US, hospitals report more requests for ECMO for teenagers and young adults and severely stretched resources.
ECMO is a vital tool but it requires highly trained staff and a huge amount of hospital resources. Patients who survive ECMO support may have long term health complications related to their critical illness.
Read more:
We’re two frontline COVID doctors. Here’s what we see as case numbers rise
Outsourcing the heart and lungs
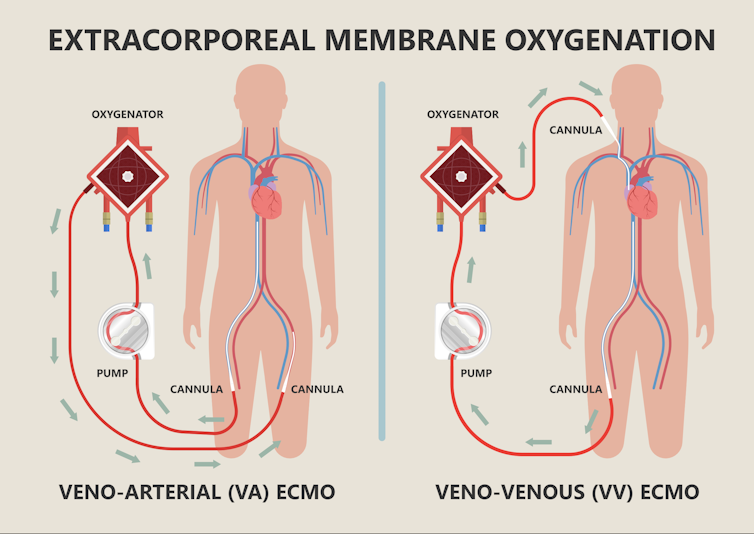
In lay terms, ECMO is a heart or lung bypass machine. A pump and artificial lung, both sitting outside the body, provide a level of support the sick organs can no longer provide. This way, the rest of the body’s functions are maintained.
The meaning of each of the letters of the ECMO acronym is:
-
Extracorporeal: outside the body
-
Membrane: the artificial lung is referred to as a “membrane”, or thin layer of material that keeps blood flowing on one side and oxygen on the other. This thin and porous membrane allows oxygen in and carbon dioxide out
-
Oxygenation: when oxygen enters the blood it is equivalent to breathing in. The process equivalent to breathing out, the removal of carbon dioxide, also occurs.
As well as the oxygenator, the ECMO machine includes cannulae – or tubing – to drain the blood from the patient and return it once oxygen has been added and carbon dioxide removed, a pump and a control panel.
ECMO evolved from cardiopulmonary bypass (heart-lung bypass) machines used to perform open heart surgery. But ECMO equipment is optimised for support lasting days to weeks rather than hours.
ECMO can be connected to the patient in two main ways: veno-venous (to replace just the function of the patient’s lungs) and veno-arterial (to do the work of both the heart and lungs).
Shutterstock
A heavy load
ECMO is the highest level of life support that can be provided, with a machine wholly or partly replacing the function of the patient’s own heart and/or lungs.
Only a small number of facilities in the world, and in Australia, are able to provide ECMO. In Australia, all ECMO services are located in large city intensive care units (ICUs), though some ECMO retrieval services can initiate ECMO support in smaller hospitals before moving patients to an ECMO ICU for ongoing care.
Highly specialised equipment and staff are required to provide ECMO.
Around-the-clock care is provided by highly trained ECMO nurses. Many ECMO ICUs have one nurse to look after the ECMO machine and another to look after the patient, who remains critically ill and usually on a full suite of other life support measures in addition to ECMO. These might include a ventilator to support the lungs, a dialysis machine to support the kidneys and many different types of drugs continuously delivered to keep the patient alive.
Medical care in the ICU is provided by large specialised teams. A broader allied health team including physiotherapists, dietitians, social workers and pharmacists help provide holistic care. Perfusionists, who specialise in extracorporeal life support, provide vital expert guidance.
Life-threatening problems with bleeding, clotting and infection are common when managing ECMO patients. Patients frequently require highly specialised support from cardiothoracic surgical teams, haematology and specialised blood bank services, radiology and interventional radiology, general surgical services, infectious diseases, cardiology, and respiratory medicine.
Some patients require weeks to months of ECMO support, which can raise ethical issues regarding resources, allocation and deaths. Some COVID patients are on ECMO for more than 100 days. The COVID pandemic has severely tested the ability of our health-care services to provide ECMO care.
Often just the beginning
A patient’s time on ECMO represents only one early phase of their critical illness recovery and, even if they survive their initial illness, most require ongoing hospital care and rehabilitation for many months afterwards. It is vital that a full suite of specialised hospital and rehabilitation services are available to maximise the patient’s chances of good quality survival.
Despite ECMO being the most complex form of life support available, the simple maxim that “prevention is better than cure” still applies.
Avoiding COVID infection by getting vaccinated, wearing a mask and paying attention to ventilation and air quality all remain vitally important to protect yourself and our healthcare system.
![]()
Greg Kelly is a Staff Specialist, Paediatric Intensive Care, Sydney Children’s Hospital Network and affiliated with OzSAGE.
Josh Ihle is Senior Intensive Care Physician and Deputy Head of Cardiothoracic ICU at the Alfred Hospital.
– ref. What is ECMO? Doctors are shocked so many ICU patients are on this advanced life support right now – https://theconversation.com/what-is-ecmo-doctors-are-shocked-so-many-icu-patients-are-on-this-advanced-life-support-right-now-171490







