Source: The Conversation (Au and NZ) – By Vasso Apostolopoulos, Professor of Immunology and Associate Provost, Research Partnerships, Victoria University

Colder weather has long been associated with coughs, colds and other respiratory illnesses. Seasonal influenza and common colds peak throughout the winter months in both hemispheres – usually around August in Australia.
Given many common colds are caused by coronaviruses, it seems logical that cases of SARS-CoV-2, the virus that causes COVID-19, would be driven upward as temperatures decline.
But while there are plausible biological explanations for why this occurs, we can’t be certain of the effect of temperature on SARS-CoV-2. There is too little data to make solid conclusions.
Behavioural factors, such as spending more time indoors where viruses are more easily transmitted, are also at play.
What does the data say?
COVID case numbers in Australia are at their highest now and were at their second-highest levels 12 months ago, in winter:
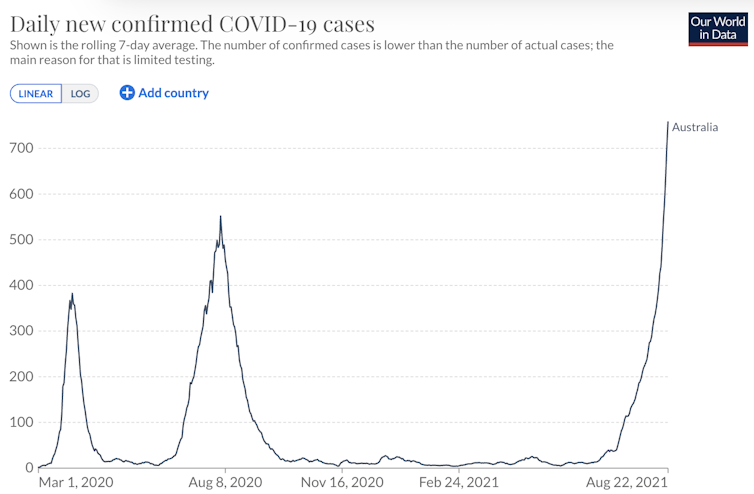
Our World In Data
But this is not true for other countries, especially those in the Northern Hemisphere. In the United Kingdom, for instance, cases peaked last winter, and then again in summer with the Delta variant:
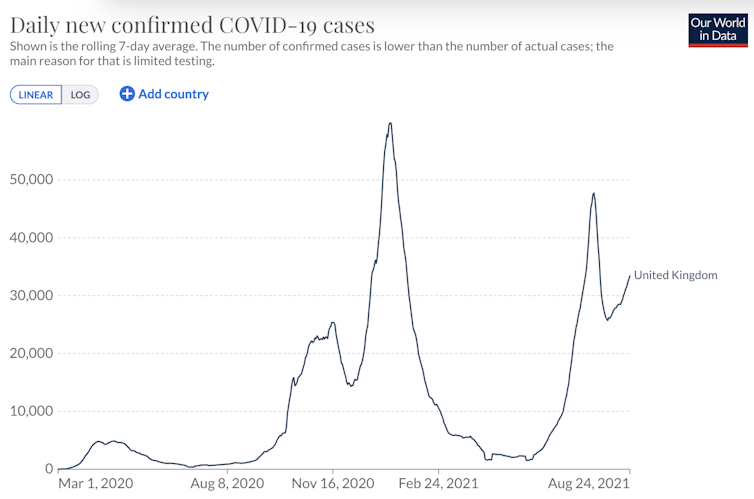
Our World In Data
Why do cases often rise in winter? Biological explanations
Coronaviruses survive longer in environments of decreased sunlight, lower temperatures and lower relative humidity.
So the amount of active virus in the environment might be greater during the winter months, and in cold, dry climates.
In environments with low humidity, there is less water vapour in the air (in other words, the air is dry), and when a COVID-19 positive person coughs, aerosolised particles stay suspended for much longer in the air. This increases the potential exposure and transmission to other people.
One study from 2020 reported a link between COVID-19 and lower humidity. The researchers noted a 1% decrease in humidity could increase the number of COVID-19 cases by 6%.
Another recent study from the United States and China found higher temperatures and higher relative humidity potentially suppressed COVID-19 transmission.
In Sydney, humidity is lowest in winter, particularly in August, and highest in summer. The same is true for most coastal areas in Australia.
Read more:
Research shows coronavirus thrives in dry air (and August is coastal Australia’s least humid month)
It’s in the air
On April 30 this year, the World Health Organization updated it guidance on how COVID-19 was transmitted:
The virus can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing or breathe. These particles range from larger respiratory droplets to smaller aerosols.
These aerosols can remain suspended in the air for up to 16 hours.
So, it’s the shared air that spreads the virus, and that’s why face masks are important.
Behavioural explanations
A range of other factors which coincide with winter are likely to have a greater impact on transmission than how the virus behaves in cold climates.
As the colder winter months arrive, we flee the outdoors, instead opting for indoor activities. Some indoor spaces – including shops, restaurants, homes – are poorly ventilated, allowing colds, flus and other respiratory illness such as COVID to spread more easily.

Shutterstock
In the northern hemisphere, winter also coincides with the holiday season, which sees significant amounts of travel, both international and domestic, and a significant uptick in large social gatherings. In the United Kingdom in January this year, this caused a significant increase in COVID-19 transmission.
It’s unlikely due to vitamin D
Another potential factor in COVID-19 transmission centres on the seasonal change in population-wide vitamin D levels. But so far, this isn’t backed up by evidence.
Vitamin D has received significant attention throughout the pandemic for a potentially protective effect against COVID-19. This was after a number of observational studies identified poorer outcomes in geographical areas with high levels of vitamin D deficiency.
Read more:
Does vitamin D ward off coronavirus? Don’t reach for the supplements yet
Other initial studies also showed lower levels of vitamin D in those diagnosed with COVID-19. This was theorised to be due to the effect of vitamin D on the immune system, preventing some of the severe inflammatory impacts of the disease, and potentially improving the ability of the individual to combat the infection.
However, larger studies where one group was given vitamin D supplements and another weren’t have thrown doubt on these relationships, particularly in those who were not deficient.
Social distance and masks matter most
While there does seem to be an increase in COVID-19 cases in the winter months, the cause of this is multi-factorial.
While certainly something for health care and policymakers to be aware of, the effect of weather and climate on COVID-19 is unlikely to have significant impact overall, and is readily countered by control measures.
Importantly, social distancing and mask use help to limit other winter viral infections such as the seasonal influenza, which was drastically reduced in winter 2020.
Paying close attention to the public health advice, particularly when indoors, should counteract any increase in COVID-19 activity in the colder months.
Read more:
Is Delta defeating us? Here’s why the variant makes contact tracing so much harder
![]()
Vasso Apostolopoulos’ COVID-19 research has received internal funding from a Victoria University research grant and from philanthropic donations
Jack Feehan does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
– ref. Rates of COVID might increase in winter, but it’s not necessarily because the virus thrives in the cold – https://theconversation.com/rates-of-covid-might-increase-in-winter-but-its-not-necessarily-because-the-virus-thrives-in-the-cold-164776




