Source: The Conversation (Au and NZ) – By James Trauer, Associate Professor, Monash University

During the pandemic, infectious disease modelling has come to prominence as never before. A plethora of models have been used to guide policy.
The models use computer programs to predict, for example, how COVID outbreaks develop and which public health measures are most likely to contain them, under different future scenarios.
Among the big questions modellers are trying to answer currently is what should Sydney’s strategy be for addressing its current Delta outbreak, to allow release from lockdown while minimising COVID-related deaths.
Different groups of researchers give different predictions. And it’s easy to be bewildered, especially if you’re in lockdown and looking for answers.
Why do answers vary?
At their best, infectious disease models should provide a way of integrating all the available information relevant to the problem at hand. This includes the characteristics of the virus circulating, the scope of the epidemic, the history of the outbreak to date, and evidence from clinical trials and other research.
We can then use this to challenge our own ideas about what the best policy response should be and develop a high-level strategy for the future.
Many of the mathematical models that have informed COVID policy across the world have been “mechanistic”. They explicitly represent the population in which the virus is transmitting and so simulate the process of susceptible people becoming infected with the virus through exposure to others.
Although many other mathematical techniques have been used during the pandemic, this approach has the advantage of being able project the outcomes of a wide range of policy responses.
Read more:
Scientific modelling is steering our response to coronavirus. But what is scientific modelling?
This approach also has several limitations. One of the most important is that tiny changes in what you feed into the model can have a huge effect on the output.
Another important consideration is that future projections inevitably represent the expected outcomes under a particular set of policy choices, which are impossible for modellers to predict.
In short, infectious disease epidemics are difficult to predict because their dynamics are volatile and dependent on the policies we choose to implement.
Let’s look at the Sydney predictions
Several groups have modelled Sydney’s lockdown recently and have shared their results with the public. These include groups at the Burnet Institute and at the universities of Sydney and Melbourne.
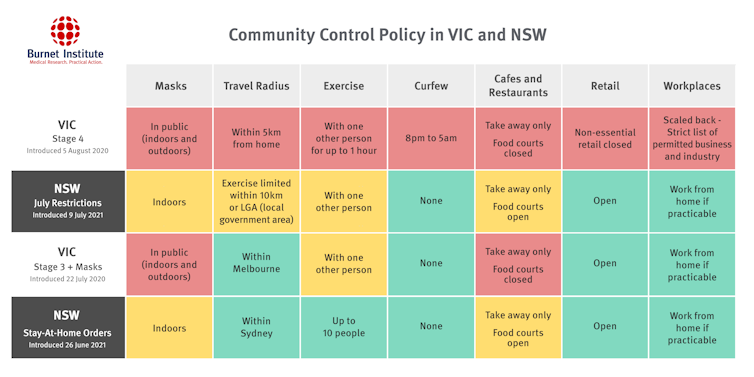
The Burnet model
The Burnet Institute simulates individuals and their characteristics and behaviours (an agent-based model). It can mimic the social networks through which individuals interact in specific settings, fundamental to how the epidemic spreads.
This approach is particularly well-suited to considering interventions that affect groups of people interacting. These include closing specific venues or activities, such as restaurants, gyms, schools or sporting events.
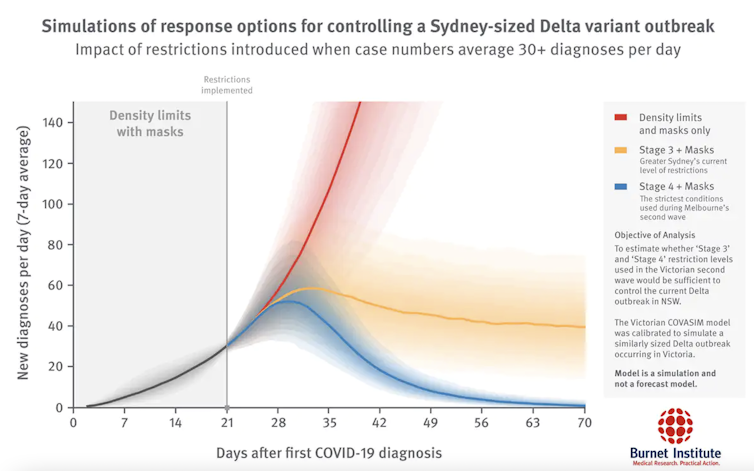
Burnet Institute
Read more:
A tougher 4-week lockdown could save Sydney months of stay-at-home orders, our modelling shows
This model, released July 12, predicted a more stringent lockdown (blue line in the chart above; something like Melbourne’s stage 4 lockdown in 2020) should be enough to drive case numbers in Sydney back down towards low levels (less than five new local cases per day) over several weeks. This would lead to elimination of the virus, allowing lockdown to lift.
Burnet Institute, July 12
University of Sydney model
The University of Sydney model is also an agent-based model, similar in several ways to the Burnet model. It builds on previous work on modelling influenza in which the researchers constructed a detailed representation of the Australian population using census data.
Along with their COVID status, the age, gender, residence and workplace of individuals is simulated, along with their commuting patterns. Various interventions are simulated, including isolating contacts of cases in quarantine, and social distancing.
The Sydney model found that unless interactions between people are reduced substantially for several weeks, the epidemic is unlikely to decline rapidly.
University of Melbourne model
The University of Melbourne model represents people or groups of people as agents who move in two-dimensional space, potentially becoming infected as susceptible agents interact with infected ones.
Because discrete individuals are represented, models like this can be used to define when the last case has recovered and elimination has been achieved.
This model generally had more optimistic findings for Sydney than the other two, with most model runs showing the epidemic dying away within two months if current restrictions or tighter are sustained. Unfortunately, case numbers already seem to be escalating beyond these predictions.
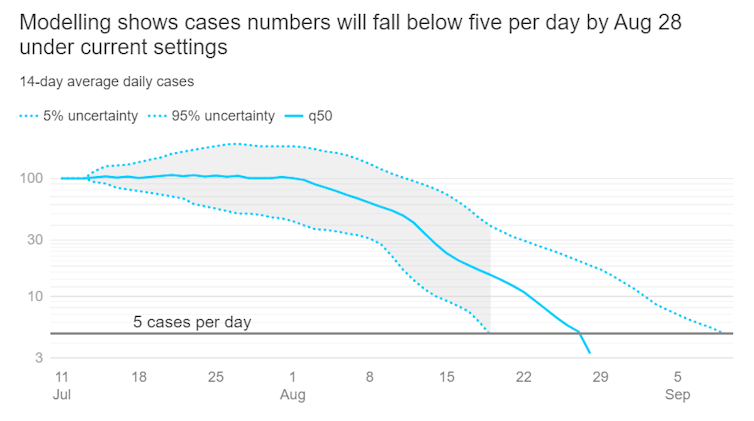
Chart: ABC news. Source: University of Melbourne
The similarities
Despite some differences in findings, we can take the following messages from these models:
-
if there had been no lockdown or if lockdowns were released now, a devastating epidemic would result
-
the public health response (including lockdown) is having a major effect in driving down transmission
-
with the current response and level of restrictions, at best it will take months to bring the epidemic fully under control
-
if restrictions are tightened considerably for at least one to two months, case numbers may decline to the point that elimination could be targeted.
Take-home message
The epidemic in Sydney is at a crossroads, with the only two feasible choices being to go hard towards elimination (as supported by all modelling groups) or to maintain manageable case numbers until vaccination begins to take effect. Current policy choices in NSW appear to prefer the latter.
The next task for modellers should be to simulate this chosen pathway and the length of lockdown it would imply.
![]()
The Epidemiological Modelling Unit at the School of Public Health and Preventive Medicine (led by James Trauer) has received funding for COVID-19 research from the NHMRC, the MRFF, the World Health Organization and the Victorian Government Department of Health and Human Services (now the Victorian Department of Health), including to produce epidemic projections during Victoria’s second wave in 2020.
– ref. When will Sydney’s lockdown end? Well, it depends who you ask – https://theconversation.com/when-will-sydneys-lockdown-end-well-it-depends-who-you-ask-165459