Source: The Conversation (Au and NZ) – By Olga Kokshagina, Researcher – Innovation & Entrepreneurship, RMIT University
How well we distribute and administer a COVID-19 vaccine will have massive health, social and economic ramifications. So attention is turning to vaccine supply chains and logistics.
Designing how best to vaccinate billions of people worldwide is complex. This is particularly so for large countries, such as Australia, where distributing vaccine to rural and remote areas is needed.
Despite numerous past pandemics and epidemics, very few studies globally have tackled the problem of designing and building an efficient vaccine distribution network. Existing studies have also not fully considered all factors affecting vaccine distribution.
So our team designed a mathematical model to test different scenarios for COVID-19 vaccine distribution, which we have submitted for publication.
What we took into account
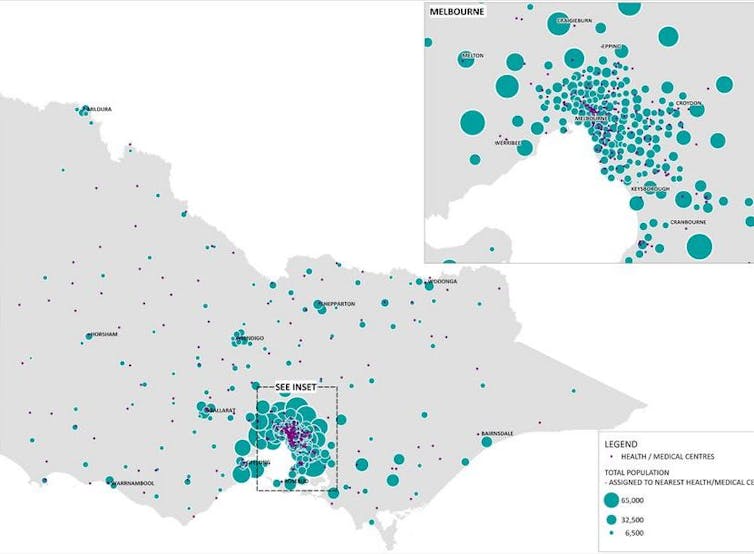
Our model looked at different ways to distribute COVID vaccine to 6.9 million Victorians, based on the number of residents predicted in 2021.We modelled this using distribution via the state’s 325 medical centres, which can be everything from big city hospitals to small medical centres in regional areas.
We assumed most vaccine distribution would be by road and enough refrigerated vehicles would be available.
We also factored into our model that certain sections of the community are at increased risk of exposure (for instance, city dwellers) and others are more susceptible to infection (for instance, aged-care residents and health-care workers). These people are not uniformly distributed around the state, affecting vaccine distribution logistics.
We then tested different scenarios to see how long vaccination would take.
Our research shows we need three key factors for success.
Read more: Scientific modelling is steering our response to coronavirus. But what is scientific modelling?
1. Medical centres need to be big enough
We calculated that if the capacity of the 325 medical centres is large enough, and if enough vaccine is available, the entire population of Victoria can be vaccinated within 60 days.
By capacity we mean the maximum number of vaccine doses each medical centre can administer. And this capacity depends on a range of factors including centres’ physical size, and having enough staff to administer vaccines.
This time frame or “target horizon” is the total number of days to vaccinate the population of Victoria. Although we have calculated this is possible within 60 days, the state or federal government will actually set this target.
Read more: Creating a COVID-19 vaccine is only the first step. It’ll take years to manufacture and distribute
To vaccinate all Victorians in 60 days, we calculated we would need a minimum of roughly 9,500 vaccine packs with 12 vaccines per pack, every day. This assumes one shot per person and adequate vaccines are available. A limited supply or a disruption to supplies might increase the administration period beyond 60 days.
If medical centres run at reduced capacity or existing capacity is not enough, this also increases the time taken to vaccinate. Conversely, if the aim is to vaccinate Victorians in under 60 days, our model suggests we need to boost our capacity to vaccinate.
This could be by using mobile vaccination units or hiring extra staff.
2. Vaccines need to be shipped between medical centres
We also show the importance of transporting vaccines between medical centres, known as transhipment. This allows medical centres short on vaccine to obtain doses from the nearest medical centres with extra supply.
Transhipment is also crucial when it comes to vaccinating the most vulnerable people. That’s because we can transfer vaccines from medical centres serving less-vulnerable populations to those with more residents in higher priority groups. Transhipment also allows us to transfer vaccines from areas with less exposure to areas of higher exposure. And it allows vaccines to reach remote areas.
However, transhipment places extra burden on road transport networks.
3. Vaccine packs need to be the right size
We also show it is important to get the vaccine pack size right. This seemingly minor detail had a significant effect on the overall period of vaccine administration.
We considered pack sizes that contain 5, 12, 20, 30 and 50 vaccines. Larger pack size significantly increases the need for transhipment between medical centres. That’s because larger packs would need to be broken up into smaller portions, then distributed to multiple medical centres.
We suggest governmental agencies carefully evaluate vaccine pack size when contracting and negotiating with vaccine manufacturers.
This is relevant to all Australia
While we used Victoria as a case study, we can apply our model to other states and territories.
In particular, the importance of pack size, transhipment between medical centres, and considering extra capacity to vaccinate in a shorter amount of time will apply in every context.
Certainly, the results for other states and territories will depend on their number of available medical centres, population size and population distribution.
Our model helps decision makers strike a balance between the cost of building extra capacity to try to achieve population vaccination in a given time scale or accepting a less costly approach that takes more time.
– ref. We modelled how a COVID vaccine roll-out would work. Here’s what we found – https://theconversation.com/we-modelled-how-a-covid-vaccine-roll-out-would-work-heres-what-we-found-150544