Source: The Conversation (Au and NZ) – By Centaine Snoswell, Research Fellow Health Economics, The University of Queensland
The expansion of telehealth services was a deliberate strategy to help reduce the risk of COVID-19 transmission between practitioners and patients, so is it working?
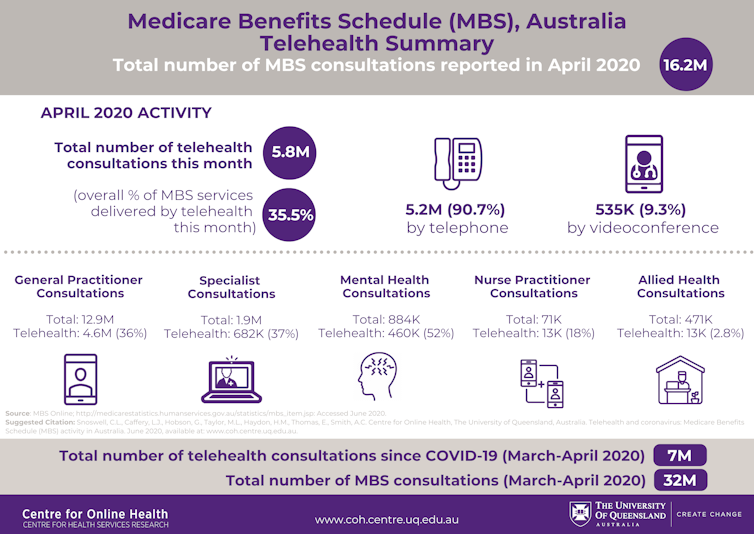
According to our analysis, the answer is that telehealth is indeed reducing the risk. Since March 2020, more than 7 million MBS-funded telehealth consultations have been reported, with the vast majority (91%) being done by telephone.
Read more: What can you use a telehealth consult for and when should you physically visit your GP?
On March 13, the federal government added new telehealth items to the Medicare Benefits Schedule, to allow health-care providers to offer both telephone and video consultations.
Before then, only Australians living outside major cities were eligible for Medicare-funded telehealth consultations, via video only. This was limited largely to medical specialist services and a very small number of GP and allied health services.In response to COVID-19, the federal government increased Medicare-funded telehealth services, including making telephone consultations available for the first time. They removed geographical constraints and increased the range of telehealth services available.
At first these expanded services were only open to vulnerable patients, such as older Australians and those with a chronic illness. But by early April, these restrictions were lifted, meaning all Australians could access Medicare-funded telehealth.

Tracking telehealth
We have been tracking the increased uptake of Medicare-funded telehealth during COVID-19. We have collected information on six different health-care discipline groups, and also compared the rates of telephone versus video consultations.
During the first six weeks after access to telehealth was expanded on March 13, 7 million consultations – or 22% of the services we examined – were delivered by telehealth.
This represents 7 million avoided face-to-face interactions between patients and health service providers, thus reducing the risk of transmission and infection.
We also found:
-
GP appointments accounted for 80% of all consultations examined. During April, GP telehealth activity was largely done by telephone but accounted for 36% of all GP consultations. This was associated with a slight reduction in face-to-face consultations – from an average of 10.5 million consultations per month before the outbreak, to 8.3 million consults in April.
-
The proportion of specialist consultations delivered via telehealth increased tenfold in March, from 0.7% in February to 7% in March. When all eligibility criteria were lifted in April, this proportion rose to 37%.
-
Although psychiatrists have provided videoconference consultations to Australians since 2002, the coronavirus outbreak prompted a steep decline in face-to-face consultations and an increase in telehealth consultations. Prior to coronavirus, around 4.5% of all consultations each month were via telehealth, this rose to 26% in April this year.
-
Mental health services provided by non-psychiatrists (including sessions provided by psychologists) showed an increase in telehealth (50% phone, 50% videoconference), and a 50% reduction in face-to-face consultations.
-
Telehealth consultations for allied health services and nurse practitioners were very limited before the pandemic. But in the six weeks from March 13, roughly 29,000 allied health and nursing telehealth consultations were reported through Medicare. Most allied health services involved video consultations, whereas nursing consultations were mainly by telephone.
Are Australians using health care more?
Is the rise in telehealth the result of patients switching from face-to-face consultations to telehealth, or are people simply accessing health care in greater numbers amid the COVID-19 pandemic? The answer varies between different parts of the health system.
Our data suggest the total number of specialist, allied heath, psychiatric and mental health consultations has stayed roughly the same. This suggests face-to-face consultations were simply being replaced by telehealth.
But for GPs and nurse practitioners, the total number of consultations rose significantly, from 10.8 million in February to 12.9 million in April. Around 90% of these telehealth consultations were delivered by phone, so the increase in activity may partly be due to the ease and simplicity of using the telephone. Alternatively, the increase may have been due to more people having health concerns amid the pandemic.

It remains to be seen whether the increase in GP and nursing consultations will continue after the pandemic, or whether it is purely related to COVID-19.
Are phone consultations adequate?
According to Medicare guidelines, telephone consultations should be offered only when video conferencing is not available. There is little doubt telephone consultations are effective in some scenarios, but we don’t yet know if they are as effective as video consultations. For this reason it has been suggested phone consultations be limited to no more than half of a practice’s telehealth provisions. This issue is one we are keen to research further.
A small survey conducted by the Consumer Health Forum found 80% of patients offered a telehealth option accepted, and 68% of patients found it better or equivalent to an in-person consultation. Public awareness of telehealth has increased rapidly, and it is likely that this awareness will help drive the continuation of telehealth.
Read more: Coronavirus has boosted telehealth care in mental health, so let’s keep it up
Telehealth is not new, but its uptake had been slow and fragmented until COVID-19 came along. The sudden telehealth switch has prompted an overnight shift in the way health care is delivered in Australia, and shown (again) that telehealth is feasible and relevant to patients’ needs. The challenge now is to make it a sustainable and routine part of health care into the future.
This is a complex task. The health workforce will need telehealth training and education; the health system will need systems to promote, refer, document and remunerate telehealth appropriately; and everyone, including patients, will need to be encouraged to view telehealth not as a stopgap or emergency option, but as an integral part of health care.
– ref. Telehealth in lockdown meant 7 million fewer chances to transmit the coronavirus – https://theconversation.com/telehealth-in-lockdown-meant-7-million-fewer-chances-to-transmit-the-coronavirus-141041




